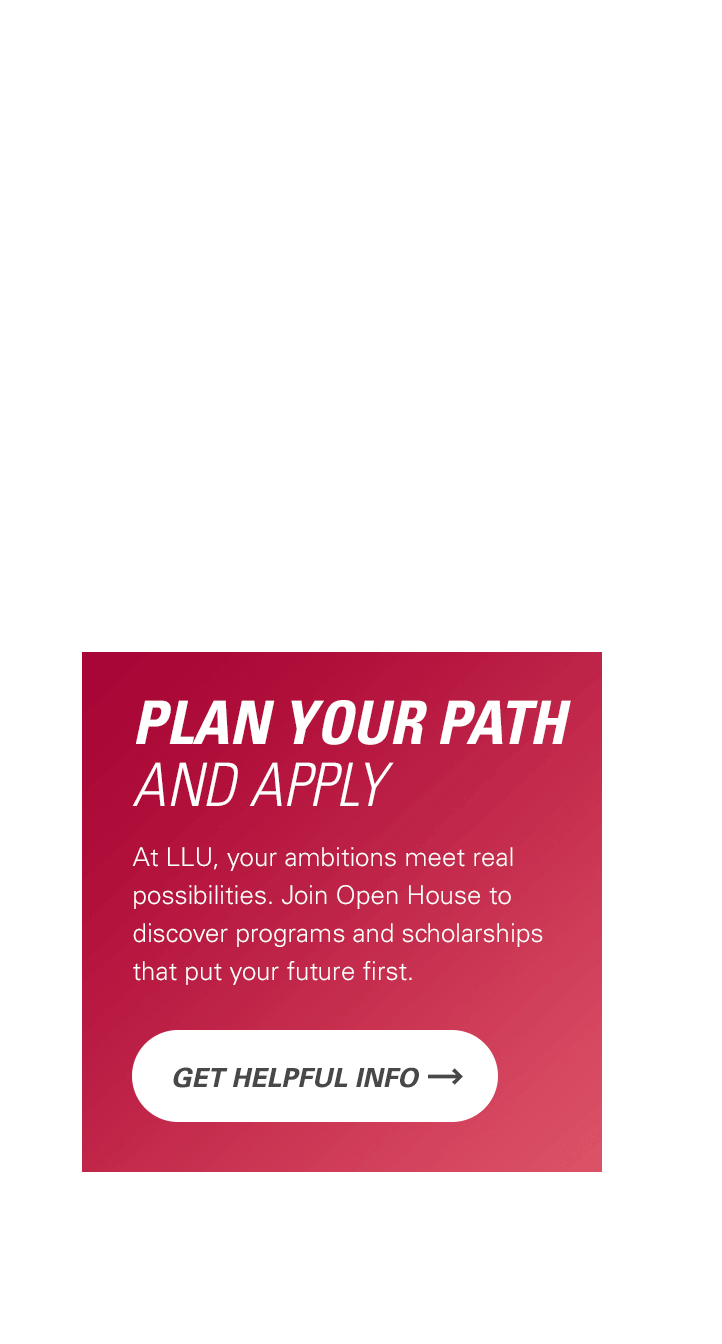
Publications
Abstract
- Shih Z, Chum PP, Bishara MA, Miot FEL, Behringer EJ. The Neurovascular Transcriptome During Alzheimer's Disease: A Central View From the Inward Rectifier K+ (KIR) Channels. 14th Across the Strait Scientific Conference on Cardiovascular Science in conjunction (ASCVS) with the 5th conference of the Asia-Pacific Undersea and Hyperbaric Medical Society (APUHMS); Tainan, Taiwan (8/25/2024). Introduction Over 55 million people worldwide live with Alzheimer disease (AD) as a major cognitive disorder due to insufficient blood flow regulation throughout the brain. Inward rectifying K+ (KIR) channel families KIR2 (Kcnj2, Kcnj12) and KIR6 (Kcnj8, Kcnj11)—as representative modulators of electrical and metabolic signaling, respectively—are abundant in cerebral vessels and fine-tune cerebral blood flow in response to metabolic demand; a process suppressed with dyslipidemia during AD. In the current study, we sought to (1) resolve neurovascular pathogenesis underlying AD; and (2) identify whether lipid disruption with cannabidiol (CBD) interferes with the molecular profile of AD onset. Our hypothesis is that AD perturbs communication among neurovascular KIR2 and KIR6 channels via RNA regulation of cholesterol and PIP2. Materials & Methods Total RNA was extracted from pial arteries, cortex, and hippocampus of male and female 3xTg-AD mice (n=3-6; 2 & 18 months old (mo)) for RNA sequencing (Zymo Research); a subset of experiments utilized dietary CBD treatment (80-100 mg/kg/day; 2 mo duration) in male animals (6.5 mo, initial AD onset). Differentially expressed genes (DEGs) and Ingenuity Pathway Analysis (Qiagen) resolved molecular pathogenesis of AD. Results Relative to 2 mo animals lacking AD pathology, 18 mo mice indicated pathways of inflammation across all tissue compartments. Further, diminished neurovascular coupling and K+ channel signaling was best marked by extracerebral pial arteries with atherosclerosis and phospholipase C signaling indicated within cortex and hippocampus respectively. Relative to vehicle controls, CBD modulated molecular networks among KIR and lipid regulators with highlighted roles for markers of neuroinflammation and AD (e.g., CXCL10, HLA-A, IGKV12-46). Conclusion Altogether, interactive molecular signaling among neurovascular inflammation, lipid, and K+ channel signaling pathways define conditions of AD pathology with CBD treatment as a potential preventative therapeutic option. (08/2024) (link)
- Behringer EJ. Neurovascular Insights into the Aging Brain & Alzheimer’s Disease: A Story of K+ Channels. 14th Across the Strait Scientific Conference on Cardiovascular Science in conjunction (ASCVS) with the 5th conference of the Asia-Pacific Undersea and Hyperbaric Medical Society (APUHMS); Tainan, Taiwan (8/24/2024). Introduction Approximately 55 million people in the world are living with Alzheimer’ disease (AD), whereby more than 95% of patients are over the age of 65; a demographic that will likely double by 2050. Cerebrovascular endothelium coordinates vasoreactivity of blood vessel networks for delivery of oxygen and nutrients throughout brain tissue in accord with metabolic demand. Our central hypothesis is that multifactorial dysregulation of endothelial K+ channel function underlies cerebrovascular aging and development of dementia. Materials & Methods To assess function of K+ channels (Ca2+-activated, KCa2.3/3.1 & inward-rectifying, KIR2), we simultaneously evaluated intracellular Ca2+ and membrane potential of intact endothelial tubes isolated from posterior cerebral arteries of male and female C57BL/6 and 3xTg-AD mice (age range, 1 to 28 mo). Comprehensive molecular screens resolved cerebrovascular non-coding & coding RNA profiles in tandem with angioarchitectural analyses. Drug interventions include Gprotein coupled receptor agonists (e.g., AT P), K+ channel openers (NS309, SKA-31), and lipid disrupting agents (e.g., methyl-β-cyclodextrin, MβCD). Results With relative conservation of cerebrovascular endothelial KCa channels throughout advancing age and AD pathology, KIR2 channel function is reduced by ∼50% and reversible with disruption of membrane cholesterol using MβCD (1 mM). Further, endothelial-specific miRNAs (miR-126-3p, miR-23a/b, miR-27a) mark onset of AD pathology and target members of the PDE, PDGF, SMAD, and VEGF families as regulators of enhanced cell growth, proliferation, and inflammation. This molecular profile aligns with structural changes (density, junctions, length) observed primarily in the cerebral vessels of 3xTg-AD animals. Conclusion The aging brain and onset of AD pathology are associated with a diminution in cerebrovascular KIR2 channel function. Altogether, our efforts reveal a need to comprehensively examine molecular mechanisms surrounding lipid signaling, inflammation, and cellular senescence interfacing with KIR channel function. In such manner, we will pursue fine-tuning of K+ channel activity as innovative therapy for perfusion of the aging brain and, in turn, prevent AD. (08/2024) (link)
- Shih ZI, Chum PP, Bishara MA, Miot FEL, Behringer EJ. MiRNA Regulation of Cerebrovascular Inwardly Rectifying K+ Channels During Onset of Alzheimer’s Disease: Role of Cholesterol and Cannabidiol Treatment. American Physiology Summit 2024 (4/4-4/7/2024). Currently, more than 6 million Americans live with Alzheimer disease (AD). Recent studies demonstrate that impaired blood flow in the brain is integral to the development of AD. Vascular inwardly rectifying K+ channels, such as KIR2.x and KIR6.x, are important for regulating vasoconstriction and vasodilation to tune cerebral perfusion in response to metabolic demand. We’ve previously identified that disruption in membrane cholesterol during advanced AD pathology restores function of KIR2.1 channels to that of young, healthy conditions or better. Additionally, we’ve identified specific microRNAs (miRNAs) in cerebral vessels that can be used to track early development of AD. In this study, we seek to understand molecular pathways stemming from miRNAs that directly or indirectly modulate activity of KIR2.x (Kcnj2, Kcnj12) and KIR6.x (Kcnj8, Kcnj11) channels. These ion channels are abundant in cerebrovascular endothelium and smooth muscle cells while particularly sensitive to dyslipidemia. We hypothesize that cerebrovascular miRNAs marking AD pathology are involved in dysregulation of inwardly rectifying K+ channels via cholesterol signaling. With employing QIAGEN’s Ingenuity Pathway Analysis (IPA), we first identified miRNAs that generally regulate each of the target genes for select KIR channels. With applying acquired knowledge of cerebrovascular miRNAs implicated in AD, we found which of these miRNAs also regulate cellular membrane cholesterol levels. Finally, we pinpointed miRNAs sensitive to cannabidiol (CBD) treatment during the development of AD as a potential therapeutic alternative to statins and cyclodextrins. In total, there are 233 miRNAs that regulate Kcnj2, 43 for Kcnj8, 203 for Kcnj11, and 177 for Kcnj12. When factoring in miRNAs that are AD-related, remaining miRNAs include nine that regulate Kcnj2, and one each for Kcnj8, Kcnj11, and Kcnj12. Remaining miRNAs that are cholesterol-related include one for Kcnj2, 43 for Kcnj8, 191 for Kcnj11, and one for Kcnj12. In general, at AD onset, CBD upregulates KIR2.2 and downregulates KIR2.1, KIR6.1, and KIR6.2 channels. CBD reversed expression of miRNAs involved in KIR2.x channel regulation in endothelial and smooth muscle/pericytes (e.g., miR-133 and miR-145) during AD onset in 3xTg-AD animals relative to wild-type controls. CBD also reverses expression of miR-129 and miR-151 to effectively upregulate genes modulating KIR6.x channels from onset of AD relative to wild-type. Altogether, we evidence specific pathways underpinning regulation of KIR2.x and KIR6.x channels in the transition from a healthy to diseased brain. This work was supported by the National Institutes of Health (R01AG073230). (05/2024) (link)
- Miot FEL, Bishara MA, Chum PP, Behringer EJ. Influence of Cholesterol Dysregulation and Cell Senescence on Hippocampal Neurovascular Integrity in Alzheimer’s Disease. American Physiology Summit 2024 (4/4-4/7/2024). The neurovascular unit (NVU) is an essential construct of cerebral blood flow control and contains neurons, astrocytes, microglia, smooth muscle, pericytes, and endothelial cells (ECs). This cellular ensemble, among other roles, balances cerebrovascular blood flow control with the metabolic demand of active neurons. Recent studies underscore the pivotal role of the NVU in Alzheimer’s disease (AD), particularly with molecular, cellular, and integrative evidence that vascular dysfunction precedes amyloid-beta (Aβ) plaque deposition. Cerebrovascular ECs are particularly vulnerable in the aging brain while central to regulation of the blood-brain barrier, hemodynamic flow, angiogenesis, and immunity. As a common characteristic of an array of cardiovascular and neurodegenerative diseases, interactions among dyslipidemia and EC health may establish cerebrovascular injury that precedes and accompanies AD. Furthermore, aberrant vascularization in the hippocampus coincides with development of mild cognitive impairment (MCI) and AD due to compromised oxygen and energy provisions in tandem with accumulation of metabolic waste and toxins. Thus, we hypothesize that interaction among cholesterol dysregulation and EC senescence signaling in the hippocampus contribute to progressive AD pathology. To test this hypothesis, we examine transgenic AD mice (3xTg-AD) demonstrating MCI (4-5 mo), presence of extracellular Aβ plaques (6-8 mo), and extracellular Aβ plaques with neurofibrillary tau tangles (≥12 mo) compared to young controls (1-2 mo). Our investigation employs an innovative tissue clearing method (iDISCO+), adapted for imaging on a confocal microscope, to probe three-dimensional vascular structure (CD31, Podocalyxin) and senescent cell aggregation (p16, β-Galactosidase) in the hippocampus. Second, Filipin III, selective blood vessel, and senescence markers are imaged in 25 μm coronal sections to examine broader spatial distribution of cholesterol around the hippocampus and cortex. Third, ex vivo blood vessel staining enables an in-depth analysis among membrane cholesterol inclusions and endothelial inward-rectifying K+ (KIR2.1) channels, an ion channel marker particularly sensitive to the distribution of membrane cholesterol while integral to cerebral blood flow control. As cholesterol dysregulation poses a significant risk to the integrity of the NVU including EC senescence and diminishment of KIR2.1 channel function, we anticipate that our results will ultimately highlight its potential role in the early to late stages of AD pathogenesis. This work was supported by the National Institutes of Health (R01AG073230). Imaging was performed in the LLUSM Advanced Imaging and Microscopy Core that is supported by NSF Grant No. MRI-DBI 0923559 and the Loma Linda University School of Medicine. (05/2024) (link)
- Chum PP, Meng S, Bishara MA, Miot FEL, Behringer EJ. Gene Expression Profile of the Mitochondrial Calcium Uniporter and Antioxidant Enzymes throughout the Brain During Alzheimer’s Disease. American Physiology Summit 2024 (4/4-4/7/2024). In 2023, there were an estimated ~6.7 million Americans ≥65 years old living with Alzheimer’s disease (AD), a prominent form of dementia. Development of AD has been associated with impaired blood flow to and throughout the brain. In turn, there is diminished delivery of oxygen and nutrients in tandem with reduced clearance of neurotoxic cellular byproducts, notably reactive oxygen species (ROS; e.g., superoxide, peroxide/hydroxyl radicals). As a primary source of cerebrovascular ROS, endothelial mitochondria become progressively dysfunctional in producing ATP relative to ROS in response to aging and cell senescence. A primary mechanism is described by enhanced Ca2+ sequestration into the mitochondrial matrix through the mitochondrial Ca2+ uniporter (MCU) complex (Mcu, Mcub, Mcur1, Micu1, Micu2, Micu3) and a resulting overproduction of ROS up to conditions of cell death. The primary antioxidants that eliminate ROS are superoxide dismutase (Sod2), catalase (Cat), and glutathione peroxidase (Gpx1). We tested the hypothesis that upregulation of the MCU complex occurs in tandem with decreasing expression of antioxidant enzymes throughout the brain during progression of AD pathology. To investigate this hypothesis, we employed a triple mutation mouse model of AD (3xTg-AD) comprising young control (YC; 1-2 mo), mild cognitive impairment (MCI; 4-5 mo), presence of extracellular amyloid-β plaques (Aβ; 6-8 mo), and extracellular amyloid-β plaques with neurofibrillary tangles composed of tau (AβT; ≥12 mo) [n ≥3 per group, males & females]. Quantitative polymerase chain reaction (qPCR), Nanostring, and/or RNA-Seq have been performed on cortex, hippocampus, cerebral vessels, cerebrovascular endothelial cells (ECs), and peripheral blood. Primary highlights of our findings for each of the AD study groups are described below. With detectable presence of all target genes throughout tissue compartments, the YC group is particularly characterized by a higher MCU complex and antioxidant expressions in cortex relative to hippocampus. During the MCI phase, the MCU complex and Cat are upregulated in ECs relative to the YC group. Upon onset of AD (Aβ stage), there is a downregulation and upregulation of MCU complex in the brain and peripheral blood respectively. Further, Gpx1 expression is upregulated in ECs in the Aβ group. Relative to YC, the MCU complex and antioxidants are downregulated in cortex but generally stable in hippocampus during AβT conditions with exception of upregulation in peroxide scavenger mRNAs Cat and Gpx1. In contrast for ECs, the MCU complex increases, while Cat and Gpx1 decrease, in the AβT group relative to YC. Altogether, these findings support an intricate expression profile of the MCU complex and key antioxidant enzymes across brain tissue and cell compartments preceding and accompanying AD pathology. A remarkable observation is that expression profiles of cerebrovascular vessels and blood indicate MCI and early onset of AD, whereas those of the cortex and hippocampus best accompany late-stage AD pathology. This research was supported by the National Institutes of Health (R01AG073230). (05/2024) (link)
- Bishara MA, Solis SR, Chum PP, Behringer EJ. Cerebrovascular miRNAs Track Early Development of Alzheimer's Disease & Target Molecular Markers of Angiogenesis and Blood Flow Regulation. American Physiology Summit 2023 (4/20-4/23/2023): Topic Group 20 (Cellular and Molecular Physiology, including Omics) & Topic Subcategory 20.20 (microRNAs: signaling and tissue remodeling). Alzheimer’s disease (AD) is the most prevalent form of dementia and currently impacts ~50 million people worldwide. AD is associated with impaired cerebrovascular function which underscores diminished delivery of blood oxygen and nutrients to and throughout the brain. Thus, we hypothesized that cerebrovascular miRNAs indicate early onset of AD pathology while corresponding to pathways of cerebrovascular growth, structure, and function. Total RNA was isolated from brain vessels of 3xTg-AD mice [Young, 1-2 mo; cognitive impairment (CI), 4-5 mo; extracellular amyloid-β plaques (Aβ), 6-8 mo; plaques + neurofibrillary tangles (AβT), 12-15 mo; n=3 males & 3 females per group]. Fifty-four cerebrovascular miRNAs detected by NanoString technology (nCounter miRNA Expression panel) were mapped to their known mRNA targets using Ingenuity Pathway Analysis. With the premise that AD is a neurovascular disorder, we sought mRNA targets along both the canonical Cardiovascular (Cardio; 15±2 targets per miRNA) and Nervous System (Neuro; 19±2 targets per miRNA) signaling strings with an overlap of 9±1 targets per miRNA among respective pathways. We found that eleven miRNAs were significantly (p<0.05) downregulated in AD (Aβ + AβT) versus Pre-AD (Young + CI) animals. In particular, let-7d, miR-99a, miR-132, and miR-181a indicated onset of AD (Aβ group) versus Young or CI. Further, miR-133a delineated CI from Young, highlighting the ability of miRNA markers to track early cerebrovascular alterations prior to AD as well. In contrast to the stability of smooth muscle-selective miRNAs (miR-143, miR-145), endothelial miRNAs (miR-23, miR-27a, miR-126) decreased with AD pathology and they target members of the PDE, PDGF, SMAD, and VEGF families. The most prominent individual mRNA markers for distinguishing onset of AD pathology while regulated by ≥3 cerebrovascular miRNAs include Slc6a1, Grin2b, Igf1r, and Smad5. The absolute difference in target overlap among respective Cardio and Neuro pathways was significantly (p<0.05) higher for all miRNAs that marked AD pathology (28±7%) relative to miRNAs stably expressed throughout (15±2%), suggesting a divergence in overall Cardio and Neuro signaling in AD relative to Pre-AD conditions. In conclusion, miRNAs selective for regulation of endothelial function and respective downstream mRNA/protein targets support a molecular basis for dysregulated cerebral blood flow regulation coupled with enhanced cell growth, proliferation, and inflammation. Accordingly, pathways associated with cerebrovascular miRNAs and their respective mRNA targets advance mechanistic and therapeutic insight for resolving early AD development. NIH Grants: R00AG047198, R56AG062169 & R01AG073230 (EJB). (05/2023) (link)
- Behringer EJ*, Hakim MA, Blackwell J, Pires PW. Endothelial KIR channel dysfunction in aged cerebral parenchymal arterioles. Experimental Biology 2022. Selected speaker for the APS Wiggers Award (Topic: Sex and Aging in the Microcirculation; Chair: David Busija) on 4/5/2022. Aging is associated with cognitive decline via mechanisms that are not fully understood. Endothelial dysfunction is known to occur in parenchymal arterioles, the bottlenecks of the cerebral microcirculation. Dilation of these arterioles is highly dependent on changes in extracellular K+ ([K+]E), caused by activity of inwardly rectifying K+ channels (KIR2) or by opening of Ca2+-activated small- and intermediate-conductance K+ channels (KCa2.3 / KCa3.1, respectively). The effects of aging on activity of these channels in the endothelium of cerebral parenchymal arterioles remain undetermined, as well as their impact on endothelium-dependent dilation. Thus, we hypothesized that advanced age will impair both KIR2 and KCa2.3 / KCa3.1 function in parenchymal arterioles of Aged mice (>24 months) when compared to Young (4-6 months). Data are means ± SEM, Young vs. Aged males and females. No sex differences were observed, thus the data were combined. Using electrophysiology, we observed that freshly-isolated endothelial cell tubes from Aged mice showed a similar hyperpolarization to the purinergic receptor agonist 2-methyl-S-ATP (1 µM), which purportedly activates the downstream effectors KIR2 and KCa2.3 / KCa3.1, than those from Young mice (Δmembrane potential (Vm): -21.0 ± 1.7 vs -23.9 ± 5.1 mV, n = 5-7), although vasodilatory responses of pressurized parenchymal arterioles were smaller (%Vasodilation: 22.4 ± 3.8 vs. 12.7 ± 3.2%, p<0.05, Student’s t-test, n = 7-6). Activity of KCa2.3 / KCa3.1 after activation by NS-309 (1 µM) was unchanged by aging, as evidenced by similar hyperpolarization (ΔVm: -36.1 ± 2.4 vs. -32.4 ± 2.2 mV, n = 13-14) and vasodilation (%Vasodilation: 16.5 ± 2.0 vs. 21.3 ± 3.2%, n = 8-6). Activation of KIR2 by 15 mM [K+]E induced a smaller hyperpolarization in Aged than Young (ΔVm: -11.0 ± 1.1 vs -6.9 ± 0.7 mV, p<0.05, Student’s t-test, n = 13-13), with a paradoxical larger vasodilation that was unchanged by endothelium removal (%Vasodilation: 10.7 ± 2.3 vs. 25.0 ± 3.6% vs. 27.3 ± 4.5, one-way ANOVA, Young endothelium intact vs. Aged endothelium intact vs Aged endothelium removed, n = 7-13-6), suggesting a compensation by smooth muscle KIR2. Lastly, spontaneous myogenic tone was higher in parenchymal arterioles from Aged mice, and endothelium removal did not further enhance myogenic tone (%myogenic tone: 25.4 ± 1.7 vs. 34.3 ± 2.3 vs 36.4 ± 3.2%, p<0.05, one-way ANOVA, Young endothelium intact vs. Aged endothelium intact vs Aged endothelium removed, n = 22-23-6). In conclusion, aging impairs endothelial KIR2 channels and increases resting myogenic tone, which may underlie vascular dysfunction and exacerbate cognitive decline. (05/2022) (link)
- Chum PP & Behringer EJ. Cerebrovascular miRNA expression profile during development of Alzheimer’s disease. Experimental Biology 2021. https://doi.org/10.1096/fasebj.2021.35.S1.02206 Alzheimer's disease (AD) is the fifth leading cause of death among Americans of age 65 years and older. Emerging evidence demonstrates the association of AD with impaired delivery of blood oxygen and nutrients to and throughout the brain. In particular, the cerebral circulation plays multiple roles underscoring optimal brain perfusion and cognition that entail moment-to-moment blood flow control, vascular permeability, and angiogenesis. With currently no effective treatment available while etiology remains obscure, discovery of novel diagnostic markers and corresponding therapeutic interventions for AD are desperately needed. Thus, to address a knowledge gap, our hypothesis was that cerebrovascular microRNA (miRNA) expression profiles corresponding to post-transcriptional regulation can provide a diagnostic map of the development of AD pathology. We screened for 600 clinically relevant miRNAs in purified brain blood vessels throughout the adult healthspan of a mouse model of AD (3xTg-AD). Using Nanostring technology, we probed for the pathological contribution of age/disease stage [young, 1-2 mo; cognitive impairment (CI), 4-5 mo; extracellular amyloid-β plaques (Aβ), 6-8 mo; plaques + neurofibrillary tangles (AβT), 12-15 mo] alongside biological sex as male vs. female (n=3 animals/group). Significant (p<0.05) downregulation of various miRNAs indicated transitions from young to CI (let-7g & let-7i, males; miR-133a & miR-2140, females) and CI to Aβ (miR-99a, males) but not from Aβ to AβT. In addition, transitions in miRNA expression from overall Pre-AD (young + CI) to AD (Aβ + AβT) conditions were detected in both males (let-7d, let-7i, miR-23a, miR-34b-3p, miR-99a, miR-132, miR-150, miR-181a) and females (miR-150, miR-539). These data demonstrate that cerebrovascular miRNAs pertaining to amyloid-β/tau regulation, remodeled vascular permeability, and enhanced angiogenesis can track early (but not late) stage development of AD pathology in a sex-based manner. Pairing such new found knowledge of vascular “signatures” of AD may yield novel theranostic approaches to maintain healthy cognition throughout adulthood. (05/2021) (link)
- Hakim MA* & Behringer EJ. Removal of membrane cholesterol selectively restores KIR channel function in brain endothelium during Alzheimer’s disease. Experimental Biology 2021. *Author & abstract won the American Physiological Society (APS) Central Nervous System (CNS) & Cell Section 2021 Research Recognition Awards. https://doi.org/10.1096/fasebj.2021.35.S1.02103 The number of Alzheimer's disease (AD) patients (~44 million worldwide; ~5.8 million Americans) continues to rise, while there is no effective treatment available and etiology remains obscure. Incidence of AD increases with aging due, in large part, to deteriorating endothelial control of blood flow throughout the brain. Further, K+ channels, particularly inward-rectifying K+ (KIR2.x) channels, are integral to endothelial function and optimal perfusion of brain parenchyma. Our group has identified reduced KIR2.x channel function as a new manifestation of endothelial “dysfunction” during aging and AD, whereas function of small- and intermediate-Ca2+-activated K+ (SKCa/IKCa) channels is stable throughout. Moreover, we reasoned that apparently deficient KIR2.x channels could be due to their aberrant interaction with plasma membrane cholesterol, a major regulator of membrane fluidity and ion channels. Hence, we tested the hypothesis that reduction of membrane cholesterol may restore KIR channel function in brain endothelium of old AD mice. Membrane potential (Vm) was measured in posterior cerebral endothelial “tubes” of female 3xTg-AD mice (16 to 19 mo; n=12) before and after mild treatment with the cholesterol-removing agent methyl-β-cyclodextrin (MβCD; 1 mM). We used elevated extracellular potassium([K+]E;15 mM) and NS309 (1 µM) to activate KIR2.x and SKCa/IKCa channels respectively. SKCa/IKCa channel function for producing hyperpolarization (more negative Vm) remains stable after MβCD treatment (ΔVm, mV; -31±1 vs. control, -33±2), revealing that SKCa/IKCa channels are not significantly impacted by membrane cholesterol. However, KIR2.x channel function is progressively restored and enhanced in a time-dependent manner following washout of MβCD (ΔVm, mV; control, -5±1; 30 min washout, -9±1; 60 min, -14±1). Altogether, our findings demonstrate that cholesterol intervention of brain endothelium selectively restores KIR2.x vs. SKCa/IKCa channel function during AD. Thus, endothelial cholesterol-KIR channel interaction is a novel therapeutic target for ameliorating cerebrovascular function to optimize perfusion of the AD brain. (05/2021) (link)
- Hakim MA & Behringer EJ. Alzheimer’s disease as a condition of accelerated aging of cerebrovascular endothelial function. Experimental Biology 2020; 4/5/2020. https://doi.org/10.1096/fasebj.2020.34.s1.03712 Currently ~5.8 million Americans have Alzheimer’s disease (AD), whereby >95% of patients are ≥65 years old. Age-related cognitive disorders including AD are associated with impaired blood flow delivery of oxygen and nutrients throughout the brain. Cerebrovascular endothelium is central to coordinating vasoreactivity of blood vessel networks for optimal cerebral blood flow. Thus we tested the hypothesis that cerebrovascular endothelial Gq-protein-coupled receptor (GPCR; P2Y) and K+ channel (KCa2.3/SK3 & KCa3.1/IK1, KIR2.1) function declines during progressive age and AD pathology. Using Fura-2 photometry (intracellular Ca2+) and sharp electrodes (membrane potential), we measured the function of endothelial tubes of posterior cerebral arteries of male and female mice (n≥5/group): C57BL/6 [young (4–6 mo), middle-aged (12–16 mo), and old (24–28 mo)] & 3xTgAD [young, no pathology (1–2 mo), mild cognitive impairment (MCI; 4–5 mo), extracellular Aβ plaques (Aβ; 6–8 mo), and Aβ plaques + neurofibrillary tangles (AβT; 12–15 mo)]. During normal aging, P2Y function in response to ATP (100 μM) was reduced in male vs. females during old age. In contrast, SKCa/IKCa channel function in response to NS309 (0.3–1 μM) decreased in old females vs. young females & old males. Activation of KIR channels to elevated extracellular K+ (15 mM KCl) decreased with advancing age regardless of sex. For 3xTgAD animals, P2Y function was maintained throughout AD pathology in females but decreased during AβT in males. SKCa/IKCa channel function was reduced in Aβ females vs. Aβ males. Further, KIR function decreased during Aβ and AβT groups regardless of sex. Altogether, AD pathology accelerates the impact of advancing age on cerebrovascular endothelium by at least 12 mo while indicating a sex-based contrast in declined function of GPCRs and K+ channels across males and females respectively. Modulation of endothelial K+ channel activity may optimize cerebral blood flow during aging and AD to prevent and treat neurodegenerative disease. Support or Funding Information This research was supported by National Institutes of Health grants R00AG047198 & R56AG062169 (EJB). (04/2020) (link)
- Hakim MA & Behringer EJ. Alzheimer’s disease as a condition of accelerated cerebrovascular aging. Bangladesh Medical Association of North America (BMANA) 11th Annual Convention (California Chapter); 2/16/2020. Alzheimer’s disease as a condition of accelerated cerebrovascular aging Md A. Hakim1, Erik J. Behringer1* 1Basic Sciences, Loma Linda University, Loma Linda, CA 92350, USA Currently ~5.8 million Americans have Alzheimer’s disease (AD), whereby >95% of patients are ≥65 years old. Age-related cognitive disorders including AD are associated with impaired blood flow delivery of oxygen and nutrients throughout the brain. Cerebrovascular endothelium is central to coordinating vasoreactivity of blood vessel networks for optimal cerebral blood flow. Thus we tested the hypothesis that cerebrovascular endothelial Gq-protein-coupled receptor (GPCR; P2Y) and K+ channel (KCa2.3/SK3 & KCa3.1/IK1, KIR2.1) function declines during progressive age and AD pathology. Using Fura-2 photometry (intracellular Ca2+) and sharp electrodes (membrane potential), we measured the function of endothelial tubes of posterior cerebral arteries of male and female mice (n≥5/group): C57BL/6 [young (4-6 mo), middle-aged (12-16 mo), and old (24-28 mo)] & 3xTgAD [young, no pathology (1-2 mo), mild cognitive impairment (MCI; 4-5 mo), extracellular Aβ plaques (Aβ; 6-8 mo), and Aβ plaques + neurofibrillary tangles (AβT; 12-15 mo)]. During normal aging, P2Y function in response to ATP (100 μM) was reduced in male vs. females during old age. In contrast, SKCa/IKCa channel function in response to NS309 (0.3-1 μM) decreased in old females vs. young females & old males. Activation of KIR channels to elevated extracellular K+ (15 mM KCl) decreased with advancing age regardless of sex. For 3xTgAD animals, P2Y function was maintained throughout AD pathology in females but decreased during AβT in males. SKCa/IKCa channel function was reduced in Aβ females vs. Aβ males. Further, KIR function decreased during Aβ and AβT groups regardless of sex. Altogether, AD pathology accelerates the impact of advancing age on cerebrovascular endothelium by at least 12 mo while indicating a sex-based contrast in declined function of GPCRs and K+ channels across males and females respectively. Modulation of endothelial K+ channel activity may optimize cerebral blood flow during aging and AD to prevent and treat neurodegenerative disease. This research was supported by National Institutes of Health grants R00AG047198 & R56AG062169 (EJB). (02/2020)
- Stoll S, Ma B, Behringer EJ, Qiu H. The valosin-containing protein resists pathological cardiac calcium overload via inhibiting mitochondrial calcium uptake. American Heart Association Council on Basic Cardiovascular Sciences 2019. Stress-induced mitochondrial calcium (Ca2+) overload is a trigger of cardiomyocyte death though the opening of mitochondrial permeability transition pore (mPTP) during cardiac ischemic injury. We previously found that the valosin-containing protein (VCP), an ATPase-associated protein, protects cardiomyocytes against stress-induced death and also inhibits mPTP opening in vitro. However, the underlying molecular mechanisms are not fully understood. Here, we tested our hypothesis that VCP protects cardiomyocytes against stress-induced mPTP opening through resisting excessive mitochondrial Ca2+ uptake. By using a cardiac-specific transgenic (TG) mouse model in which VCP is overexpressed by 3.5 folds in the hearts, we found that, under the pathological extra-mitochondrial Ca2+ overload (10-70μM), Ca2+ entered into cardiac mitochondriawas much lessin VCP TG mice compared to little-matched WT mice, subsequently preventing mPTP opening and ATP depletion under the Ca2+ challenge. Mechanistically, overexpression of VCP in the heart results in post-translational protein degradation of the mitochondrial Ca2+ uptake protein 1 (MICU1), an activator of the mitochondria Ca2+ uniporter (MCU) which is responsible for mitochondrial calcium uptake. Together, our results reveal a new regulatory role of VCP in cardiac mitochondrial Ca2+ homeostasis and unlocks the potential mechanism by which VCP confers its cardioprotection. (10/2019) (link)
- Jullienne A, Obenaus A, Lee JB, Behringer E; for the MODEL-AD Consortium. Lifespan magnetic resonance imaging of novel mouse models of Alzheimer’s disease: phenotyping and comparisons to healthy aging. Society for Neuroscience 2019; 10/22/2019 (morning session). Topic: C.02. Alzheimer's Disease and Other Dementias; Program #/Poster #: 473.01/E20. The Model Organism Development and Evaluation for Late-Onset Alzheimer’s Disease (MODEL-AD) consortium has been established to develop the next generation of Alzheimer’s disease (AD) models based on human data. As these models are developed, they are rigorously characterized using genomic, histological, electrophysiological and behavioral measures. Magnetic resonance imaging (MRI) provides multiple contrasts to probe the healthy aging brain of C57BL/6J mice and AD mouse models as they exhibit progressive onset of the disease. Several AD mouse models are being assessed, including 5xFAD (a commonly used model of familial AD) and human amyloid beta (Aß) knock-in mice, wherein the human Aß which forms the characteristic fibrillar plaques of AD is expressed under the murine endogenous promoter. All MODEL-AD mice are compared to age-matched littermates (C57BL/6J) mice at 4, 8, 12 and >18mo (N=8-9/sex/age). Mice underwent high-resolution MRI to assess their phenotype: T2-weighted and susceptibility-weighted imaging (11.7T) were used for brain region volumetric analysis and quantitative analysis of Aß plaque load, and diffusion tensor imaging (DTI, 9.4T) was used to analyze white matter tracts. Emerging data found significant volumetric reductions (~6%) in cerebrum volumes between 8mo-old female C57BL/6J and age-matched 5xFAD mice. Hippocampal volumes were significantly reduced in 4mo-old males but not females when comparing C57BL/6J to 5xFAD mice. DTI metrics that report tissue features, such as fractional anisotropy, radial, axial and mean diffusivity will evaluate the progressive alterations in AD mouse models over their lifespan. Preliminary tractography mapping circuits from hippocampal CA1 to the subiculum found sex-specific differences in the number and density of tracts (streamlines) in healthy 4mo C57BL/6J mice. Such novel sex differences will be analyzed in our novel AD mouse models as well as age-matched healthy control mice. In summary, phenotyping using multimodal MRI can identify altered brain connectivity and regional tissue metrics across the mouse lifespan in healthy aging and in AD models. These MRI approaches can lead to clinically translatable tools for assessment of AD progression in human patients. For more information, see model-ad.org. (10/2019) (link)
- Hakim MA, Buchholz JN, Behringer EJ. Alteration of Calcium and Electrical Dynamics in Cerebrovascular Endothelium During Development of Alzheimer’s disease. Experimental Biology 2019; 4/7/2019. This abstract was picked for the Microcirculatory Presidents’ Poster Reception (Section: Development, Angiogenesis, and Signaling; Poster #21). https://doi.org/10.1096/fasebj.2019.33.1_supplement.518.5 Alzheimer's disease (AD) is a progressive neurodegenerative disease and the most common cause of dementia characterized by a decline in cognitive function among the elderly. Currently, ~5.7 million Americans are living with AD and this number will increase to ~14 million by 2050. Age-related AD alters blood flow to the brain and is associated with cerebral hypoperfusion, due in part, to impaired vascular endothelial function. However, it is unknown whether AD pathology impacts the biophysical functions of key cerebral vascular G-protein-coupled receptors (GPCRs) and K+ channels (KCa2.3 or SKCa, KCa3.1 or IKCa) that govern blood flow via an electrical vasodilatory pathway known as endothelium-derived hyperpolarization (EDH). Thus, we tested the hypothesis that cerebrovascular endothelial purinergic receptors and Ca2+-activated K+ channels become functionally dysregulated during progression of AD. We used the triple mutation mouse model of AD (3xTgAD) to examine endothelium isolated from posterior cerebral arteries in young control (YC; 1–2 mo), amyloid-β plaques (Aβ; 6–8 mo), and plaques + neurofibrillary tangles (Aβ+Tau; ≥ 12 mo); n ≥ 3 male & n ≥ 3 female mice/group. Intracellular calcium concentration ([Ca2+]i) and membrane potential (Vm) were simultaneously measured using Fura-2 photometry and sharp electrodes (pH 7.4, 37°C). EDH was demonstrated by an increase in [Ca2+]i (ΔF340/F380 ≥ 0.3) concomitant with ΔVm ≥ −10 mV in response to the P2Y agonist ATP (100 μM, 3 min). Membrane hyperpolarization to ATP during Aβ+Tau vs. YC decreased (ΔVm, mV; YC: −20±4, Aβ: −17±2, Aβ+Tau: −13±3) while [Ca2+]i responses were maintained. In contrast, hyperpolarization increased during Aβ and Aβ+Tau (ΔVm, mV; YC: −29±3, Aβ: −36±2, Aβ+Tau: −38±3) during direct activation of SKCa/IKCa alone with SKA-31 (10 μM, 5 min). Finally, Δ[Ca2+]i and ΔVm responses to hydrogen peroxide (H2O2; 200 μM, 20 min) in young control animals were greater by > 40% as compared to Aβ & Aβ+Tau. These data suggest coupling of endothelial SKCa/IKCa function with Ca2+ signaling is reduced and adaptation to oxidative stress occurs during the development of AD. Altogether, endothelial K+ channel function may be directly calibrated for optimal cerebral blood flow to maintain a healthy brain with aging while helping to prevent neurodegenerative disease. Support or Funding Information This research is supported by Loma Linda University School of Medicine new faculty start-up funds and National Institutes of Health grants R00AG047198 & R56AG062169 (EJB). (04/2019) (link)
- Nye PP & Behringer EJ. Genetic Expression Profile of Cerebrovascular Endothelium During Development of Alzheimer’s Disease. Experimental Biology 2019; 4/7/2019. https://doi.org/10.1096/fasebj.2019.33.1_supplement.518.1 In 2018 alone, seven-hundred thousand Americans of age 65 years and older will have a form of Alzheimer's disease (AD) by the end of their lives. Emerging evidence demonstrates the association of AD with impaired delivery of blood oxygen and nutrients to and throughout the brain. Cerebral arteries coordinate vasodilation through endothelium-derived hyperpolarization (EDH); sequentially entailing stimulation of G protein-coupled receptors (GPCRs), increases in intracellular Ca2+, activation of small- and intermediate-conductance Ca2+-activated K+ channels (SKCa/IKCa), and spread of negative intracellular charge (“hyperpolarization”) through cell-to-cell gap junctions. Thus, we tested the hypothesis that the genetic expression of EDH vasodilatory components may decline during progression of age-related AD in mouse cerebrovascular endothelium. We used the triple mutation mouse model of AD (3xTgAD) to examine cerebrovascular genetic profiles for young control (YC; 1 to 2 mo), mild cognitive impairment (MCI; 4 to 5 mo), amyloid-β plaques (Aβ; 6 to 8 mo), and plaques + neurofibrillary tangles (Aβ+Tau; ≥12 mo); 3 male and 3 female mice/group. Quantitative polymerase chain reaction (qPCR) and RNA sequencing were used to examine genetic expression of isolated cerebral artery endothelium and purified brain vessels respectively. The qPCR results demonstrate mixed expression of respective isoforms of purinergic receptors as indicated by no changes for P2ry1 (transcript for P2Y1) but ~35% and ~65% upregulation of P2ry2 (P2Y2) during Aβ and Aβ+Tau respectively. In contrast, the expression of ion channel mRNA in the form of major K+ channels (Kcnn3/Kcnn4, SKCa/IKCa & Kcnj2, inward rectifying KIR2.1) and transient receptor potential channels (Trpv4, TRPV4) remains relatively stable throughout the life of the animal. Further, with the exception of Gja1 (Cx43), the expression of connexins composing gap junctions (Gja4, Cx37 & Gja5, Cx40) increased by ≥ 20% during Aβ and Aβ+Tau. Finally, RNAseq data and pathway analysis demonstrate a >two-fold upregulation of genes integral to cardiovascular remodeling during Aβ+Tau vs. YC. Overall, these data indicate profound genetic alterations underlying cerebral blood vessel function corresponding to moment-to-moment regulation of blood flow and chronic maintenance of vascular structure. Pairing new found knowledge of vascular “signatures” with developmental phases of AD may offer unprecedented opportunities to maintain a healthy mind throughout the entirety of a standard lifespan (~80 to 100 years). Support or Funding Information This research is supported by Loma Linda University School of Medicine new faculty start-up funds and National Institutes of Health grants R00AG047198 & R56AG062169 (EJB). (04/2019) (link)
- Hakim MA, Buchholz JN, Behringer EJ. Altered intracellular calcium reactivity of cerebral artery endothelial tubes with advancing age. Society for Neuroscience 2017; 11/13/2017, 325.20/NN1) Intracellular Ca2+ ([Ca2+]i) signaling in cerebral artery endothelial cells coordinates smooth muscle cell relaxation facilitating cerebral blood flow. However, studies of endothelial function are limited by the presence of confounding factors (e.g., perivascular nerves, blood flow, hormones) arising from intact blood vessel applications. Also, isolated cells in culture manifest significantly altered morphology and ion channel expression relative to physiological conditions. The aim of the current study was to characterize intact vascular endothelium freshly isolated (≤1 hr of being within the animal) from middle and posterior cerebral arteries of Young (4-7 mo), Middle (13-16 mo), and Old (24-27 mo) male and female C57BL/6 mice (n ≥ 5; continuous superfusion of PSS at pH 7.4 & 37°C). Using Fura-2 photometry (~100 cells), we tested the hypothesis that aging increases the magnitude of cerebral endothelial [Ca2+]i responses in response to a physiological G-protein coupled receptor agonist (ATP) and the oxidizing agent H2O2. A cerebral endothelial tube varied in length from 0.5 to 3 mm, whereby diameter was not significantly altered with age (Young: 108±12 µm, Middle: 105±7 µm, Old: 120±7 µm; mean ± SEM) or gender. With resting [Ca2+]i in the range of 100 nM to 300 nM, increases in [Ca2+]i were typically up to ~500 nM during treatment with the purinergic receptor agonist ATP (100 µM, 5 min) and highest at µM concentrations following H2O2 (200 µM, 15 min). With general trends (P>0.05) for greater increases in females vs. males across age groups, ?[Ca2+]i to ATP and H2O2 peaked at middle age (P<0.05; ≈ two-fold vs. Young) and decreased by ≈30% (P>0.05) in Old. These data suggest that middle age sets the stage for enhanced [Ca2+]i signaling, thereby increasing the Ca2+ homeostasis burden of internal organelles (ER and mitochondria). Further, intracellular measurements of Vm during respective treatments demonstrated hyperpolarization of membrane potential (Vm) across groups consistent with activation of small- and intermediate- Ca2+-activated K+ channels (or SKCa/IKCa) with NS309 (?Vm of -5 mV to -50 mV from a resting Vm of ≈-30 mV to -40 mV). As [Ca2+]i and oxidative signaling modulates SKCa/IKCa activity and vasodilation, these findings provide insight into endothelial cell regulation of cerebral blood flow with advancing age and the potential development of neurodegenerative disease. This work has been supported by NIH grant R00AG047198 (EJB) (11/2017) (link)
- Jafarnejad M, Behringer EJ, Scallan JP, Davis MJ, Segal SS, Moore Jr. JE. Mathematical Model of Calcium and Electrical Dynamics in Lymphatic Endothelium. Experimental Biology 2016. FASEB J. 30:726.9, 2016. Contraction of collecting lymphatic vessels is essential for immunity and tissue fluid balance. The underlying role of lymphatic endothelium is unknown. In contrast to blood vessels, lymphatic endothelial cell tubes (LECTs; mouse popliteal fossae) do not govern membrane potential (Vm) via small- and intermediate-conductance Ca2+ activated K+ channels (SKCa/IKCa). Consequently, despite similarity in the intracellular Ca2+ ([Ca2+]i) response to acetylcholine (1 μM) (i.e., rapid initial peak followed by secondary “plateau” phase), depolarization of Vm (ΔVm: 29±4 mV, n=11 LECTs) ensues in contrast to classic hyperpolarization in blood vessels (ΔVm: −38±3 mV, n=4 popliteal arteries). To further resolve the contribution of respective ions and channel [e.g. transient receptor potential (TRP)] currents to LECT depolarization, we adapted mathematical models of [Ca2+]i dynamics and ion fluxes (e.g., Hodgkin-Huxley). Modeling reproduced [Ca2+]i responses and accompanying depolarization observed experimentally. Furthermore, depolarization required a combination of Na+ and Ca2+ influx via cation membrane channels (e.g., TRP canonical & vanilloid 4, Orai) during the plateau phase. Roles of other ions (e.g., K+, Cl−) and respective channels (e.g., inward-rectifying K+ & volume-regulated anion) were also apparent. Altogether, the absence of SKCa/IKCa function during robust Na+ and Ca2+ mobilization determines the electrical activity of lymphatic endothelium. Such novel cellular signaling may regulate the efficacy of lymphatic muscle cell activity to control lymph transport during health while disruption of these interactions may contribute to disease. (04/2016) (link)
- Behringer EJ. Impact of aging on calcium and electrical signaling in microvascular endothelium. Ninth Annual Division of Aging Biology New Investigator’s Forum. NIH campus, Bethesda, MD, June 18-19, 2015. (06/2015)
- Behringer EJ & Segal SS. Modulating calcium entry into microvascular endothelium by controlling membrane potential during submaximal muscarinic receptor activation. Annual meeting of the Biophysical Society 2015. Biophys J. 108(2):p105a, 2015. Vascular smooth muscle cell relaxation and vasodilation are coupled to a rise in endothelial cell [Ca2+]i and hyperpolarization. However, the role of membrane potential (Vm) in regulating endothelial cell [Ca2+]i remains controversial. To test the hypothesis that Vm can govern Ca2+ entry into endothelial cells in accord with its electrochemical gradient, we evaluated [Ca2+]i using Fura-2 photometry (F340/F380) while controlling Vm using intracellular current injection. Intact endothelial tubes (width: 60 μm, length: ≤ 1 mm) were freshly isolated from superior epigastric arteries of C57BL/6 mice (n≥7; 32°C, pH 7.4). Endothelial cells were electrically coupled to each other through gap junctions and lacked inherent voltage-sensitive ion channel activity as indicated by linearity (R2 = 0.990±0.002) of the current-voltage relationship throughout the Vm range of ≈-80 mV to +10 mV during current injection (±0.5 to 5 nA). In the absence of receptor activation, Vm was −37±1 mV and [Ca2+]i did not change with hyperpolarization or depolarization. In contrast, during submaximal activation of muscarinic (Gq protein-coupled) receptors (GPCRs) with acetylcholine (100 nM; ∼EC50), [Ca2+]i increased with hyperpolarization to −60±1 mV and decreased with depolarization to −28±2 mV. The effect of membrane hyperpolarization on [Ca2+]i was abolished following removal of [Ca2+]o (control [Ca2+]o = 2 mM) and reduced by half in endothelium isolated from TRPV4-/- mice during Vm > −50 mV. Thus, submaximal stimulation of GPCRs enables physiological changes in Vm to modulate Ca entry through voltage-insensitive ion channels in the plasma membrane of native microvascular endothelial cells. (Support: NIH grants R37-HL041026, 5T32-AR048523, 1K99-AG047198) (01/2015) (link)
- Behringer EJ & Segal SS. Hyperpolarization enhances calcium influx into endothelium of resistance arteries during muscarinic receptor activation: role of TRPV4 channels. 11th International Symposium on Resistance Arteries (ISRA; Banff, Alberta, Canada, 9/2014). Session ID: PS1-42; Abstract: ISRA76. Published in J Vasc Res. 2014:51 Suppl 2:1-156. PMID: 25501311; doi: 10.1159/000369652 A rise in endothelial [Ca2+]i initiates hyperpolarization to promote smooth muscle relaxation. In turn, hyperpolarization may enhance endothelial [Ca2+]i through a mechanism that remains to be defined. To test the hypothesis that hyperpolarization augments Ca2+ influx into endothelial cells of resistance arteries, endothelial tubes (width, 60 µm; length, ≤ 1 mm) were isolated from superior epigastric arteries of adult (3-6 months) male C57BL/6 mice (n≥7). Fura-2 photometry was evaluated during intracellular injection of negative current (-0.5 to -5 nA; each for 20s) to control Vm. Under resting conditions (32 °C, pH 7.4, [Ca2+]o = 2 mM), membrane potential (Vm) was -35±3 mV. Negative current hyperpolarized cells (-1 nA, -45±2mV; -2 nA, -55±2mV; -3 nA, -65±1mV; -4 nA, -73±1mV; -5 nA, -79±2mV) without altering [Ca2+]i (e.g., F340/F380 = 0.70 at rest, 0.71±0.02 during -5 nA). For negative current injected during ACh treatment (100 nM, ~EC50), [Ca2+]i increased with the magnitude of hyperpolarization (?F340/F380 & ?Vm; for -1 nA, 0.06±0.01 & -11±1mV; -2 nA, 0.12±0.01 & -20±1mV; -3 nA, 0.15±0.01 & -28±2mV; -4 nA, 0.18±0.01 & -34±2 mV; -5 nA, 0.19±0.01 & -41±2mV). This effect of hyperpolarization on [Ca2+]i was reduced by half in endothelial tubes isolated from TRPV4-/- mice [e.g., for -5 nA: ?F340/F380=0.09±0.03 with ?Vm = -41±6 mV) and abolished upon removing [Ca2+]o. Thus Vm governs Ca2+ entry during submaximal activation of ion channels that include TRPV4. Enhancing endothelial Ca2+ influx through hyperpolarization can augment vasodilation. (Support: NIH grants R37-HL041026, 5T32-AR048523, 1K99AG047198) (09/2014) (link)
- Behringer EJ & Segal SS. Modulating Ca2+ entry into endothelial tubes by controlling membrane potential during muscarinic receptor activation. Experimental Biology 2014. FASEB J 28: 664.7, 2014. Coupling of intracellular Ca2+ [Ca2+]i to hyperpolarization of endothelial cells underlies smooth muscle cell relaxation in resistance vessels. Whether membrane potential (Vm) influences [Ca2+]i levels in the endothelium remains controversial. To resolve the impact of Vm on Ca2+ influx, Fura-2 photometry was evaluated during intracellular current injection (-5 to +5 nA; 20 s pulses) to control Vm of endothelial tubes (width, 60 µm; length, ? 1 mm) freshly isolated from superior epigastric arteries of adult (4-6 mo) male C57BL/6 mice (n?4). Relative to resting Vm (-40±2 mV), current injection hyperpolarized (Vm in mV; -1 nA: -52±2, -3 nA: -64±2, -5 nA: -79±2) and depolarized (+1 nA: -33±1, +3 nA: -13±2, +5 nA: 8±3) cells. Under resting conditions, changing Vm did not affect [Ca2+]i (e.g., F340/F380 = 0.68±0.03 at rest and -5 nA). However, during exposure to acetylcholine (ACh; 100 nM, ~EC50), the plateau phase of the [Ca2+]i response was either enhanced [?F340/F380 & ?Vm (mV); -1 nA: 0.07±0.02 & -10±1; -3 nA: 0.16±0.02 & -23±2; -5 nA: 0.21±0.02 & -38±1] or reduced (+1 nA: -0.08±0.02 & 11±2; +3 nA: -0.18±0.03 & 28±3; +5 nA: -0.34±0.03 & 49±4) according to voltage amplitude and polarity (P<0.05). These effects of ACh and ?Vm were abolished in the absence of extracellular Ca2+ (2 mM). Thus Vm can modulate Ca2+ entry during submaximal activation of ion channels that enable Ca2+ influx in accord with the electrochemical driving force. Grant Funding Source: Supported by R37-HL041026 & 5T32-AR048523 (04/2014) (link)
- Behringer EJ, Socha MJ, Westcott EB and Segal SS. Sustained calcium release and hyperpolarization in microvascular endothelium with advanced age. Joint meeting of the North American Vascular Biology Organization (NAVBO) and the Microcirculatory Society (MCS), October 20-24, 2013. (10/2013) (link)
- Behringer EJ & Segal SS. Altered electrical reactivity of endothelial tubes with aging: Role of mitochondria and Ca2+-activated K+ channels. Experimental Biology 2013. FASEB J. 27:679.1, 2013. Hyperpolarization of endothelial cells (ECs) is integral to coordinating smooth muscle cell relaxation throughout resistance networks and endothelial function is compromised with aging. Aberrations in mitochondrial function may contribute to endothelial dysfunction however little is known of such effects with aging in the microcirculation. We tested (P<0.05) whether disrupting the proton gradient across the inner mitochondrial membrane (IMM) altered plasma membrane potential (Vm) in endothelial tubes (width, 60 μm; length, 1–3 mm) freshly isolated (bath pH, 7.4; 32°C) from superior epigastric arteries of Young (4–6 mo) and Old (24–26 mo) male C57BL/6 mice. The IMM proton ionophore FCCP (10 nM-10 μM) depolarized Young ECs progressively (from resting Vm of −33±2 mV to −17±2 mV; n=5). In contrast, FCCP (10 nM-10 μM) hyperpolarized Old ECs progressively (from −42±4 to −67±3 mV; n=5) which was abolished by SKCa/IKCa channel blockade with apamin (Ap, 300 nM) + charybdotoxin (ChTx, 100 nM). In Old, 300 nM FCCP hyperpolarized ECs by −12±1 mV and this reversed to 9±1 mV depolarization with Ap+ChTx (n=4). Despite no effect on Vm of Young, BKCa channel activation (NS1619, 30 μM) hyperpolarized Old ECs by −13±1 mV (n=6). We hypothesize that changes in endothelial function with aging reflects mitochondrial dysregulation of SKCa/IKCa channels with acquired BKCa channel activity. (R01HL086483, R37HL041026, F32HL110701) (04/2013) (link)
- Behringer EJ, Scallan JP, Davis MJ, and Segal SS. Depolarization of collecting lymphatic endothelium with acetylcholine or TRPV4 activation. Experimental Biology 2013. FASEB J. 27:678.3, 2013. Smooth muscle cells of collecting lymphatic vessels undergo coordinated contractions to propel lymph centrally. Whether endothelial-derived hyperpolarization [via activation of small- and intermediate-conductance Ca2+ activated K+ channels (SKCa/IKCa)] shown in blood vessels is manifest in governing lymphatic function has not been established. To test this possibility, lymphangions dissected from mouse popliteal fossae were treated to yield intact lymphatic endothelial cell tubes (LECTs; width: ~50μm; length: ~500 μm) for intracellular recording (bath pH 7.4; 30°C). Resting membrane potential (Vm) of LECTs was −60±5 mV and depolarized (P<0.05) to −49±5 mV with BaCl2 (100 μM; n=6). Activation (NS309, 1 μM) or blockade [apamin (300 nM) + charybdotoxin (100 nM)] of SKCa/IKCa did not alter Vm (n=4). Acetylcholine (ACh, 1 μM) or GSK (TRPV4 channel agonist; 100 nM) depolarized LECTs by 29±7 and 49±4 mV, respectively (P<0.05; n=4 each). Thus blockade of inward-rectifying K+ channels and agents promoting Ca2+influx (via TRPV4) as well as release from the endoplasmic reticulum (ACh) evoke LECT depolarization that is facilitated by lack of functional SKCa/IKCa expression. With myoendothelial coupling, endothelium-derived depolarization may coordinate contraction of lymphatic smooth muscle cells and thereby determine the effectiveness of lymph transport. (NIH R37HL041026, R01HL086483, F32HL110701, R01HL089784) (04/2013) (link)
- Behringer EJ & Segal SS. Aging restricts electrical signaling along endothelial tubes via enhanced activation of SKCa/IKCa channels: role for oxidative stress. Annual meeting of the Biophysical Society 2013. Biophys J. 104(2):493a, 2013. Electrical conduction in cellular networks is governed by gap junction patency between cells and the open state of membrane ion channels. In light of endothelial cell (EC) dysfunction with aging, we determined whether aging altered electrical signaling. Intact endothelial tubes (width: ≈60μm; length ≥ 2mm) isolated from superior epigastric arteries of Young (4-6 months) and Old (24-26 months) male C57BL/6 mice were studied using dual intracellular microelectrodes. Separation distance between sites of current injection and membrane potential (Vm) recording was 50-2000μm. A reduction in electrical length constant (Δ) from 1630 (Young) to 1320μm (Old) accompanied an increase in restingVm from Young (-28±1mV) to Old (−36±1mV) (n≥9; P<0.05). With similar pEC50 values and maximum Vm responses to acetylcholine (ΔVm Young: 7.3±0.1, −38±3mV; Old: 7.2±0.1, −39±1mV), the conduction amplitude (CA; ΔVm/nA current injection) for intercellular electrical signaling was less (P<0.05) in Old vs. Young (at 500 μm: 5.9±1 vs. 8.9±1 mV/nA; n=6). Despite similar hyperpolarization (∼-35 mV) to direct activation of calcium-activated K+ channels (SKCa/IKCa; KCa2.3 and KCa3.1) with NS309 (1μM), the reduction in CA was greater (P<0.05) in Young vs. Old (−6±1 vs.-4±1 mV/nA; n≥7). Inhibiting SKCa/IKCa (apamin+charybdotoxin) restored conduction in Old to that of Young (at 500 μm:∼10 mV/nA; n=6). To investigate a role for oxidative stress, H2O2 (200 μM) increased Vm to EK (≈-90mV) and impaired CA by ≥ 90% (n=8) in Young; these effects were blocked by apamin+charybdotoxin (n=6). Catalase (500 U/ml) depolarized resting Vm from −38±1 to −28±1mV and increased CA by ≈30% in Old (n=7; P<0.05). Thus restricted spread of electrical signals along endothelium of Old reflects enhanced current dissipation through open SKCa/IKCa in response to oxidative stress. (Support: NIH R01-HL086483, R37-HL041026, F32-HL110701) (01/2013) (link)
- Behringer EJ. Young Investigator Session: Aging impairs electrical conduction along endothelial tubes via activation of KCa channels by reactive oxygen species. Joint meeting of the British Microcirculation Society & the Microcirculatory Society, Inc. 2012. (07/2012) (link)
- Behringer EJ & Segal SS. Tuning electrical conduction along endothelial cell tubes via Ca2+-activated K+ channels. Experimental Biology 2012. FASEB J. 26:1058.12, 2012. Electrical conduction along coupled cells reflects low axial resistance (ra) of gap junction channels (GJCs) and high plasma membrane resistance (rm) to current flow. Manipulating GJCs alters conducted vasomotor responses but little is known of how conduction may be governed by membrane ion channel activation. We hypothesized that Ca2+-activated K+ channels (SKCa/IKCa) can tune rm to regulate electrical conduction along endothelial cell (EC) tubes (width, 60 μm; length, ≥ 2 mm) isolated from feed arteries of C57BL/6 mouse skeletal muscle (n = 6–10 males). Using dual simultaneous intracellular microelectrodes, membrane potential (Vm) was uniform along EC tubes (−25 ± 2 mV) and propidium iodide dye injected into one EC spread throughout neighbouring ECs. Conduction amplitude (CA = ΔVm at Site 2/nA current injected at Site 1) decreased with electrode separation distance (CA = 11, 8, 6, 4, 3 ± 1 mV/nA at 50, 500, 1000, 1500, 2000 μm). The SKCa/IKCa activator NS309 (1μM) reduced length constant [λ = (rm/ra)½] from 1360 ± 80 to 840 ± 60 μm (P<0.05). With electrode separation = 500 μm, NS309 from 0.01 to 10 μM increased Vm from −28 ± 1 to −81 ± 1 mV and abolished CA while dye transfer was maintained; blocking SKCa/IKCa (300 nM apamin + 100 nM charybdotoxin) increased CA by ~30% (P<0.05). We conclude that the effectiveness of electrical conduction can be tuned through SKCa/IKCa activation. (NIH R37HL041026, R01HL086483, F32HL110701) (04/2012) (link)
- Behringer EJ & Segal SS. Aging impairs electrical conduction along resistance artery endothelium via enhanced signal dissipation through KCa channels. Experimental Biology 2012. FASEB J. 26:861.2, 2012. Aging results in endothelial cell (EC) dysfunction yet little is known of how intercellular transmission of electrical signals is affected. We hypothesized that aging impairs electrical conduction via current dissipation through Ca2+-activated K+ channels (SKCa/IKCa). EC tubes (width: 60 μm; length: ≥ 2 mm) isolated from Young (3–6 mo, n ≥ 10) and Old (24–26 mo, n ≥ 8) superior epigastric arteries of male C57BL/6 mice were studied using dual simultaneous intracellular microelectrodes placed at separation distances of 50–2000 μm. Membrane potential (Vm) was greater in Old (−35 ± 2) vs. Young (−26 ± 1 mV; P < 0.05). Conduction amplitude (CA; ΔVm at Site 2/nA current injected at Site 1) was less in Old vs. Young (at 500 μm: 6 ± 1 vs. 10 ± 1 mV/nA; P < 0.05). SKCa/IKCa activation (1 μM NS309) increased Vm similarly for Old (Δ = −32 ± 2) and Young (Δ = −35 ± 2 mV) and the reduction in CA was greater in Young vs. Old (−6 ± 1 vs. −4 ± 1 mV/nA; P < 0.05). SKCa/IKCa inhibition (300 nM apamin + 100 nM charybdotoxin) evoked greater depolarization in Old (Δ = 14 ± 2) vs. Young (Δ = 7 ± 1 mV; P < 0.05) and the resulting increase in CA was greater in Old (45 ± 7%) vs. Young (22 ± 6%; P < 0.05) which restored conduction in Old to that of Young (both = 10 ± 1 mV/nA). We conclude that aging impairs electrical conduction along the endothelium by increasing signal dissipation through enhanced SKCa/IKCa activation. (NIH R01HL086483, R37HL041026, F32HL110701) (04/2012) (link)
- Behringer EJ, Socha MJ, Jackson WF, Segal SS. IKCa/SKCa channels modulate electrical conduction along microvascular endothelial tubes. Peer-reviewed abstract accepted by the 10th International Symposium on Resistance Arteries (ISRA; Rebild Bakker, Denmark, 5/2011). (05/2011) (link)
- Behringer EJ, Polo-Parada L, Jackson WF, Segal SS. Glycyrrhetinic acid derivatives block hyperpolarization concomitant with intercellular coupling along microvascular endothelial tubes. Experimental Biology 2011. FASEB J. 25:817.5, 2011. Cell-to-cell conduction of hyperpolarization through gap junctions along endothelial cells promotes smooth muscle cell hyperpolarization and vasodilation. Using intact endothelial tubes (width, ~60 μm; length, 700–2000 μm) isolated from mouse abdominal feed arteries and devoid of smooth muscle cells, we tested the hypothesis that purported gap junction blockers carbenoxolone (CBX, 100 μM) or β-glycyrrhetinic acid (βGA, 30 μM) would inhibit conducted hyperpolarization. Dual simultaneous intracellular recording confirmed stability of membrane potential (Vm) at 2 sites separated by 500 μm (Vm1 = −24±2, Vm2 = −23 ± 1 mV; n=14). Injecting negative current (−0.5 to −5 nA) at Site 1 produced hyperpolarization at Site 2 (−3 to −30 mV). Calculated transfer resistance (TR = ΔVm at Site 2/current injected at Site 1) was 6.2 ± 0.6 MΩ (n=9). Either CBX or βGA eliminated ΔVm at Site 2 (TR=0; n=6, P<0.05); αGA (100 μM) had no effect (n=3). Remarkably, CBX or βGA also inhibited hyperpolarization to either 3 μM acetylcholine [from −39 ± 2 (control) to −3 ± 1 mV (treatment; n=18, P<0.05)] or to 1 μM NS309 [from −33 ± 4 to −1 ± 1 mV (n = 5, P<0.05)]. These findings illustrate that glycyrrhetinic acid derivatives purported to block gap junctions concomitantly block endothelial cell hyperpolarization. (Support: HL056786, HL041026, HL086483) (04/2011) (link)
- Behringer EJ, Leite LD, Buchholz NE, Keeney MG, Pearce WJ and Buchholz JN. Development and long-term hypoxia alters calcium-induced calcium release in sheep cerebrovascular neurons. Society for Neuroscience 2008 (482.4/RR37). Stimulation-evoked release of calcium from intracellular stores, called calcium induced calcium release (CICR) is necessary for the proper function of superior cervical ganglia (SCG) neurons and is mediated via ryanodine receptors (RyR). We measured the contribution of CICR to electrical field stimulation (EFS)-evoked intracellular calcium ([Ca2+]i) transients (6-24 pulses, 3 Hz), in isolated fura-2 loaded SCG cells, from normoxic and long-term high altitude hypoxic (LTH) near-term fetal and adult sheep. In addition, we measured the cellular levels of RyR and their modulators, neuronal nitric oxide synthase (nNOS) and cyclic adenosine diphosphate ribose (cADPR), using ELISA assay to measure the protein levels and a fluorometric assay to measure cADPr levels. EFS-evoked [Ca2+]i transients in SCG from normoxic fetuses were significantly greater than the other groups tested. The effect of ryanodine to block CICR and reduce EFS-evoked [Ca2+]i transients was greatest in the fetal normoxic group over the entire stimulation range (6-24 pulses), and the effect of ryanodine was completely lost in LTH fetal SCG cells. In SCG cells from adult normoxic and LTH animals, ryanodine significantly decreased EFS-evoked [Ca2+]i transients only at the supermaximal stimulation (18 to 24 pulses). Levels of RyR2 and RyR3 declined only with development and cellular levels of cADPR normalized to nNOS levels were greatest in normoxic fetal SCG and declined with development and LTH. These data suggest that the sensitivity of CICR to EFS and its contribution to EFS-evoked [Ca2+]i transients declines with development and is lost in fetal SCG neurons during LTH. The decline in CICR during development may in part be due a decline in the levels of RyR2 and RyR3. However, during LTH the loss of CICR is not necessarily due to changes in RyR levels but may be in part due to the efficiency of synthesis of RyR modulators such as cADPr. In addition, in terms of [Ca2+]i signaling there appears to be an accelerated or premature maturation of the fetus towards that of the adult with LTH. (11/2008) (link)
- Behringer EJ, Vanterpool CK, Pearce WJ and Buchholz JN. Impact of advancing age on caffeine-mediated sensitization of calcium release in superior cervical ganglion cells. Experimental Biology 2008. FASEB J. 22:1126.7, 2008. In vascular sympathetic neurons calcium-induced calcium release (CICR) is mediated by ryanodine receptors (RyR) and contributes to the magnitude of stimulation-evoked intracellular calcium ([Ca2+]i) transients. Furthermore, this process can be sensitized with RyR agonists such as caffeine. In this study we assessed the contribution of CICR to the magnitude of electric field stimulation (EFS)-evoked [Ca2+]i transients. We measured EFS-evoked changes in [Ca2+]i in isolated fura-2 loaded superior cervical ganglion (SCG) cells, from F-344 rats aged 6, 12, and 24 months. EFS was delivered over a range of 3 to 24 pulses (3Hz) in the absence and presence of 5mM caffeine. Maximal EFS-evoked increases in [Ca2+]i significantly increased from 6-12 months and then declined at 24 months, suggesting that CICR as a component of the EFS-evoked [Ca2+]i transient declines with age. However, most interestingly, caffeine significantly increased EFS-evoked [Ca2+]i transients over the entire stimulation range (3–24 pulses) in all age groups. In addition, caffeine decreased the number of pulses to achieve ½ maximal EFS-evoked [Ca2+]i in all age groups. Taken together, the data suggest that with advancing age although the contribution of CICR to EFS-evoked [Ca2+]i transients may decline with age, some of this function can be reclaimed in the presence of RyR agonists such as caffeine. Supported in part by NIH HED P01 #31226 (03/2008) (link)
- Buchholz JN, Vanterpool CK, Pearce WJ and Behringer EJ. Advancing age alters the contribution of release of calcium from internal stores to stimulation-evoked calcium transients to stimulation-evoked influx in rat superior cervical ganglia. Experimental Biology 2007. FASEB J. 21:A1350, 2007. In vascular adrenergic neurons the release of calcium from SER stores known as calcium induced calcium release (CICR) plays a role in determining the magnitude and shape of stimulation-evoked intracellular calcium ([Ca2+]i) transients. The release of calcium is triggered by activation of ryanodine receptor (RYR) channels. We measured electric field stimulation (EFS)-evoked [Ca2+]i transients in isolated fura-2 loaded superior cervical ganglion (SCG) cells from F-344 rats aged 6, 12 and 24 months. 50 square-wave pulses of EFS (5Hz) were delivered using a Grass stimulator via platinum electrodes. The current was ramped from 50–300 mA in the absence (control) and presence of the RYR antagonist, ryanodine (100 μM) to block release of calcium from SER stores. EFS-evoked changes in peak and rate of rise of [Ca2+]i significantly declined by 43% and 59% respectively in SCG cells from 24 month-old animals as compared to 6 and 12 months (P<0.05 by ANOVA). Following the addition of ryanodine, EFS-evoked changes in peak and rate of rise of [Ca2+]i significantly declined by 22% and 25% respectively only in SCG cells from 6 and 12 month-old animals with no effect at 24 months (P<0.03 by paired T-test). In addition, following blockade of CICR the dynamics of EFS-evoked [Ca2+]i transients in young cells is similar to old. These data suggest that in SCG cells there is an age-related decline in the contribution of CICR in determining the magnitude and shape of EFS-evoked [Ca2+]i transients. Supported in part by NIH HED P01 #31226 (04/2007) (link)
- Behringer EJ, Vanterpool CK, Pearce WJ and Buchholz JN. Late maturation and advancing age alter the contribution of release of calcium from internal stores to stimulation-evoked calcium transients. Society for Neuroscience 2006 (80.5/KK12). Release of calcium from SER stores plays an important role in neuronal cell signaling and shapes stimulation-evoked intracellular calcium ([Ca2+]i) transients. The release of calcium is triggered by activation of ryanodine receptor (RYR) channels. We measured electric field stimulation (EFS)-evoked [Ca2+]i transients in isolated fura-2 loaded superior cervical ganglion (SCG) cells from F-344 rats aged 6, 12 and 24 months. 50 square-wave pulses of EFS (5Hz) were delivered using a Grass stimulator via platinum electrodes. The current was ramped from 50-300 mA in the absence (control) and presence of the RYR antagonist, ryanodine (10 µM) to block release of calcium from SER stores. Peak [Ca2+]i transients vs current were plotted and the current producing one half maximal peak [Ca2+]i (IC50) was determined for each cell using Origin Software. The IC50 in the absence of ryanodine (control) varied significantly with age in SCG cells from 6, 12 and 24 month old animals and were 153 ±11.2, 119 ±9.2 and 200 ± 20 mA respectively (P<0.05 by ANOVA). Ryanodine significantly increased the IC50 in SCG cells from 6 and 12 (P<0.05, paired t-test) but not in 24 month-old animals, and were 162 ±10, 154 ±7.7 and 220 ±16.6 mA respectively. These data suggest that during late maturation, SCG cells are more sensitive to EFS due to an increase in release of calcium from the SER and this sensitivity declines with senescent aging. In addition, the contribution of SER calcium release in shaping EFS-evoked [Ca2+]i transients increases with late maturation and declines with senescence. These data are consistent with our recent published results demonstrating that RYR3 expression and modulation is altered with late maturation and senescent aging. (10/2006) (link)
Scholarly Journals--Published
- Chum PP, Bishara MA, Solis SR, Behringer EJ. Cerebrovascular miRNAs track early development of Alzheimer’s disease & target molecular markers of angiogenesis and blood flow regulation. J Alzheimer’s Dis. 99(s2): S187-S234, 2024. PMID: 37458037; PMCID: PMC10787821; doi: 10.3233/JAD-230300 Background: Alzheimer's disease (AD) is associated with impaired cerebral circulation which underscores diminished delivery of blood oxygen and nutrients to and throughout the brain. In the 3xTg-AD mouse model, we have recently found that > 10 cerebrovascular miRNAs pertaining to vascular permeability, angiogenesis, and inflammation (e.g., let-7d, miR-99a, miR-132, miR-133a, miR-151-5p, and miR-181a) track early development of AD. Further, endothelial-specific miRNAs (miR-126-3p, miR-23a/b, miR-27a) alter with onset of overall AD pathology relative to stability of smooth muscle/pericyte-specific miRNAs (miR-143, miR-145). Objective: We tested the hypothesis that cerebrovascular miRNAs indicating AD pathology share mRNA targets that regulate key endothelial cell functions such as angiogenesis, vascular permeability, and blood flow regulation. Methods: As detected by NanoString nCounter miRNA Expression panel for 3xTg-AD mice, 61 cerebrovascular miRNAs and respective mRNA targets were examined using Ingenuity Pathway Analysis for canonical Cardiovascular (Cardio) and Nervous System (Neuro) Signaling. Results: The number of targets regulated per miRNA were 21±2 and 33±3 for the Cardio and Neuro pathways respectively, whereby 14±2 targets overlap among pathways. Endothelial miRNAs primarily target members of the PDE, PDGF, SMAD, and VEGF families. Individual candidates regulated by≥4 miRNAs that best mark AD pathology presence in 3xTg-AD mice include CFL2, GRIN2B, PDGFB, SLC6A1, SMAD3, SYT3, and TNFRSF11B. Conclusion: miRNAs selective for regulation of endothelial function and respective downstream mRNA targets support a molecular basis for dysregulated cerebral blood flow regulation coupled with enhanced cell growth, proliferation, and inflammation. (05/2024) (link)
- Behringer EJ. The impact of aging on vascular ion channels: Perspectives and knowledge gaps across major organ systems. Am J Physiol Heart Circ Physiol. 325(5): H1012-H1038, 2023. PMID: 37624095; PMCID: PMC10908410; doi: 10.1152/ajpheart.00288.2023 Individuals aged ≥65 yr will comprise ∼20% of the global population by 2030. Cardiovascular disease remains the leading cause of death in the world with age-related endothelial "dysfunction" as a key risk factor. As an organ in and of itself, vascular endothelium courses throughout the mammalian body to coordinate blood flow to all other organs and tissues (e.g., brain, heart, lung, skeletal muscle, gut, kidney, skin) in accord with metabolic demand. In turn, emerging evidence demonstrates that vascular aging and its comorbidities (e.g., neurodegeneration, diabetes, hypertension, kidney disease, heart failure, and cancer) are "channelopathies" in large part. With an emphasis on distinct functional traits and common arrangements across major organs systems, the present literature review encompasses regulation of vascular ion channels that underlie blood flow control throughout the body. The regulation of myoendothelial coupling and local versus conducted signaling are discussed with new perspectives for aging and the development of chronic diseases. Although equipped with an awareness of knowledge gaps in the vascular aging field, a section has been included to encompass general feasibility, role of biological sex, and additional conceptual and experimental considerations (e.g., cell regression and proliferation, gene profile analyses). The ultimate goal is for the reader to see and understand major points of deterioration in vascular function while gaining the ability to think of potential mechanistic and therapeutic strategies to sustain organ perfusion and whole body health with aging. (11/2023) (link)
- Polk FD, Hakim MA, Silva JF, Behringer EJ, Pires PW. Endothelial KIR2 channel dysfunction in aged cerebral parenchymal arterioles. Am J Physiol Heart Circ Physiol. 325(6): H1360-H1372, 2023. PMID: 37801044; PMCID: PMC10907073; doi: 10.1152/ajpheart.00279.2023. Comment in “To err, KIR2 that is, on the side of vasodilation in aging” by Ricardo B. de Paula, Camilla F. Wenceslau, and Cameron G. McCarthy. Am J Physiol Heart Circ Physiol 325(6): H1415-H1417, 2023. PMID: 37861649; doi: 10.1152/ajpheart.00670.2023. Aging is associated with cognitive decline via incompletely understood mechanisms. Cerebral microvascular dysfunction occurs in aging, particularly impaired endothelium-mediated dilation. Parenchymal arterioles are bottlenecks of the cerebral microcirculation, and dysfunction causes a mismatch in nutrient demand and delivery, leaving neurons at risk. Extracellular nucleotides elicit parenchymal arteriole dilation by activating endothelial purinergic receptors (P2Y), leading to opening of K+ channels, including inwardly-rectifying K+ channels (KIR2). These channels amplify hyperpolarizing signals, resulting in dilation. However, it remains unknown if endothelial P2Y and KIR2 signaling are altered in brain parenchymal arterioles during aging. We hypothesized that aging impairs endothelial P2Y and KIR2 function in parenchymal arterioles. We observed reduced dilation to the purinergic agonist 2-methyl-S-ADP (1 µM) in arterioles from Aged (>24-month-old) mice when compared to Young (4-6 months of age) despite similar hyperpolarization in endothelial cells tubes. No differences were observed in vasodilation or endothelial cell hyperpolarization to activation of small- and intermediate-conductance Ca2+-activated K+ channels (KCa2.3 / KCa3.1) by NS309. Hyperpolarization to 15 mM [K+]E was smaller in Aged than Young mice, despite a paradoxical increased dilation in Aged arterioles to 15 mM [K+]E that was unchanged by endothelium removal. KIR2 Inhibition attenuated vasodilatory responses to 15 mM [K+]E and 1 µM 2-me-S-ADP in both Young and Aged arterioles. Further, we observed a significant increase in myogenic tone in Aged parenchymal arterioles, which was not enhanced by endothelium removal. We conclude that aging impairs endothelial KIR2 channel function in the cerebral microcirculation with possible compensation by smooth muscle cells. (10/2023) (link)
- Dietrich A, Behringer EJ, Taylor MS, Sonkusare SK. Editorial: Transient receptor potential channels (TRP): signal transduction. Front Mol Biosci. 10: 1201614, 2023. PMID: 37187892; PMCID: PMC10176508; doi: 10.3389/fmolb.2023.1201614 (04/2023) (link)
- Hakim MA & Behringer EJ (2022). KIR channel regulation of electrical conduction along cerebrovascular endothelium: Enhanced modulation during Alzheimer’s disease. Microcirculation. e12797. PMID: 36577656 Objective Endothelial cell (EC) coupling occurs through gap junctions and underlies cerebral blood flow regulation governed by inward-rectifying (KIR) channels. This study addressed effects of KIR channel activity on EC coupling before and during Alzheimer's disease (AD). Methods Intact EC tubes (width: ~90-100 μm; length: ~0.5 mm) were freshly isolated from posterior cerebral arteries of young Pre-AD (1-3 months) and aged AD (13-18 months) male and female 3xTg-AD mice. Dual intracellular microelectrodes applied simultaneous current injections (±0.5–3 nA) and membrane potential (Vm) recordings in ECs at distance ~400 μm. Elevated extracellular potassium ([K+]E; 8-15 mmol L-1; reference, 5 mmol L-1) activated KIR channels. Results Conducted Vm (?Vm) responses ranged from ~-30 to 30 mV in response to -3 to +3 nA (linear regression, R2≥0.99) while lacking rectification for charge polarity or axial direction of spread. Conduction slope decreased ~10-20% during 15 mmol L-1 [K+]E in Pre-AD males and AD females. 15 mmol L-1 [K+]E decreased conduction at lower thresholds in AD animals (~±20 mV) versus Pre-AD (~±25 mV). AD increased (~10-15%) conducted hyperpolarization during 8-12 mmol L-1 [K+]E. Conclusions Brain endothelial KIR channel activity modulates bidirectional spread of vasoreactive signals with enhanced regulation of EC coupling during AD pathology. (01/2023) (link)
- Jullienne A, Quan R, Szu JI, Trinh MV, Behringer EJ, Obenaus A (2022). Progressive vascular abnormalities in the aging 3xTg-AD mouse model of Alzheimer’s disease. Biomedicines. 10(8):1967. PMID: 36009514; PMCID: PMC9405684 Vascular dysfunction and structural abnormalities in Alzheimer's disease (AD) are known to contribute to the progression of the pathology, and studies have tended to ignore the role of the vasculature in AD progression. We utilized the 3xTg-AD mouse model of AD to examine individual cerebral vessels and the cortical vascular network across the lifespan. Our vessel painting approach was used to label the entire cortical vasculature, followed by epifluorescence microscopy. The middle cerebral artery (MCA) tree was assessed with confocal microscopy, and a new method was developed to assess branching patterns as a measure of aging-related changes. We found that vascular remodeling was profoundly altered at 4-6 months of age, when the 3xTg-AD mouse is known to transition to cognitive impairment and Aβ deposition in both sexes. Analysis of vascular features (density, junctions, length) of the MCA territory highlighted sex-dependent differences across the 3xTg-AD mouse lifespan, with no alterations in branching patterns. Our current cerebrovascular angioarchitectural analyses demonstrate progressive alterations in individual cortical vessels, as well as in the vascular network of the cortex. These new findings advance our understanding of brain anatomy and physiology in the 3xTg-AD mouse, while potentially identifying unique diagnostic signatures of AD progression. (08/2022) (link)
- Hakim MA, Pires PW, Behringer EJ (2022). Isolation and functional resolution of arteriolar endothelium of mouse brain parenchyma. J Vis Exp. e63463. PMID: 35343953; PMCID: PMC9154351 Cerebral blood flow is conveyed by vascular resistance arteries and downstream parenchymal arterioles. Steady-state vascular resistance to blood flow increases with decreasing diameter from arteries to arterioles that ultimately feed into capillaries. Due to their smaller size and location in the parenchyma, arterioles have been relatively understudied and with less reproducibility in findings than surface pial arteries. Regardless, arteriolar endothelial cell structure and function—integral to the physiology and etiology of chronic degenerative diseases—requires extensive investigation. In particular, emerging evidence demonstrates that compromised endothelial function precedes and exacerbates cognitive impairment and dementia. In the parenchymal microcirculation, endothelial K+ channel function is the most robust stimulus to finely control the spread of vasodilation to promote increases in blood flow to areas of neuronal activity. This paper illustrates a refined method for freshly isolating intact and electrically coupled endothelial “tubes” (diameter, ~25 μm) from mouse brain parenchymal arterioles. Arteriolar endothelial tubes are secured during physiological conditions (37 °C, pH 7.4) to resolve experimental variables that encompass K+ channel function and their regulation, including intracellular Ca2+ dynamics, changes in membrane potential, and membrane lipid regulation. A distinct technical advantage versus arterial endothelium is the enhanced morphological resolution of cell and organelle (e.g., mitochondria) dimensions, which expands the usefulness of this technique. Healthy cerebral perfusion throughout life entails robust endothelial function in parenchymal arterioles, directly linking blood flow to the fueling of neuronal and glial activity throughout precise anatomical regions of the brain. Thus, it is expected that this method will significantly advance the general knowledge of vascular physiology and neuroscience concerning the healthy and diseased brain. (03/2022) (link)
- Chum PP, Hakim MA, Behringer EJ (2022). Cerebrovascular microRNA expression profile during early development of Alzheimer’s disease in a mouse model. J Alzheimer’s Dis., 85(1): 91-113. PMID: 34776451; PMCID: PMC9169494 Abstract. Background: Emerging evidence demonstrates association of Alzheimer’s disease (AD) with impaired delivery of blood oxygen and nutrients to and throughout the brain. The cerebral circulation plays multiple roles underscoring optimal brain perfusion and cognition entailing moment-to-moment blood flow control, vascular permeability, and angiogenesis. With currently no effective treatment to prevent or delay the progression of AD, cerebrovascular microRNA (miRNA) markers corresponding to post-transcriptional regulation may distinguish phases of AD. Objective: We tested the hypothesis that cerebrovascular miRNA expression profiles indicate developmental stages of AD pathology. Methods: Total RNA was isolated from total brain vessel segments of male and female 3xTg-AD mice [young, 1–2 mo; cognitive impairment (CI), 4–5 mo; extracellular amyloid- plaques (A), 6–8 mo; plaques+neurofibrillary tangles (AT), 12–15 mo]. NanoString technology nCounter miRNA Expression panel for mouse was used to screen for 599 miRNAs. Results: Significant (p < 0.05) downregulation of various miRNAs indicated transitions from young to CI (e.g., let-7g & miR-1944, males; miR-133a & miR-2140, females) and CI to A (e.g., miR-99a, males) but not from A to AT. In addition, altered expression of select miRNAs from overall Pre-AD (young + CI) versus AD (A + AT) were detected in both males (let-7d, let-7i, miR-23a, miR-34b-3p, miR-99a, miR-126-3p, miR-132, miR-150, miR-151-5p, miR-181a) and females (miR-150, miR-539). Altogether, at least 20 cerebrovascular miRNAs effectively delineate AD versus Pre-AD pathology. Conclusion: Using the 3xTg-AD mouse model, these data demonstrate that cerebrovascular miRNAs pertaining to endothelial function, vascular permeability, angiogenesis, inflammation, and A/tau metabolism can track early development of AD. (01/2022) (link)
- Hakim MA & Behringer EJ (2021). Methyl-beta-cyclodextrin restores KIR channel function in brain endothelium of female Alzheimer’s disease mice. J Alzheimer’s Dis Rep., 5(1): 693-703. PMID: 34755043; PMCID: PMC8543374 Abstract. Background: As the sixth-leading cause of death in the United States, Alzheimer’s disease (AD) entails deteriorating endothelial control of blood flow throughout the brain. In particular, reduced inward-rectifying K+ (KIR) channel function in animal models of aging and AD compromises endothelial function and optimal perfusion of brain parenchyma. Deficient endothelial KIR channels may result from aberrant interaction with plasma membrane cholesterol as a primary regulator of membrane fluidity and ion channels. Objective: We tested the hypothesis that mild methyl--cyclodextrin (MCD) treatment to reduce membrane cholesterol may restore endothelial KIR channel function in brain endothelium of old AD mice. Methods: Membrane potential was continuously measured in isolated endothelial tubes from posterior cerebral arteries of young (1 to 3 months) and old (16 to 19 months) female 3xTg-AD mice before and after mild treatment with the cholesterolremoving agent MCD (1 mmol/L). Elevated extracellular potassium ([K+]E; 15 mmol/L) and NS309 (1 mol/L) activated KIR and Ca2+-activated K+ (SKCa/IKCa) channels respectively before and after MCD treatment. Results: SKCa/IKCa channel function for producing hyperpolarization remained stable regardless of age group and MCD treatment (Vm: ∼–33 mV). However, as deficient during AD, KIR channel function was restored (Vm: –9 ± 1 mV) versus pre-MCD conditions (–5 ± 1 mV); a progressive effect that reached –14 ± 1 mV hyperpolarization at 60 min following MCD washout. Conclusion: In female animals, MCD treatment of brain endothelium selectively restores KIR versus SKCa/IKCa channel function during AD. Thus, the endothelial cholesterol-KIR channel interface is a novel target for ameliorating perfusion of the AD brain. (09/2021) (link)
- Hakim MA, Nye-Chum P, Buchholz JN, Behringer EJ (2020). Aging alters cerebrovascular endothelial GPCR and K+ channel function: Divergent role of biological sex. J Gerontol A Biol Sci Med Sci. 75(11):2064-2073. PMID: 31760422; PMCID: PMC7709862 Abstract Age-related dementia entails impaired blood flow to and throughout the brain due, in part, to reduced endothelial nitric oxide signaling. However, it is unknown whether sex affects cerebrovascular Gq-protein-coupled receptors (GPCRs) and K+ channels underlying endothelium-derived hyperpolarization (EDH) during progressive aging. Thus, we simultaneously evaluated intracellular Ca2+ ([Ca2+]i) and membrane potential (Vm) of intact endothelial tubes freshly isolated from posterior cerebral arteries of young (4-6 mo), middle-aged (12-16 mo), and old (24-28 mo) male and female C57BL/6 mice. Purinergic receptor function (vs. muscarinic) was dominant and enhanced for [Ca2+]i increases in old females versus old males. However, Ca2+-sensitive K+ channel function as defined by NS309-evoked Vm hyperpolarization was mildly impaired in females versus males during old age. This sex-based contrast in declined function of GPCRs and K+ channels to produce EDH may support a greater ability for physiological endothelial GPCR function to maintain optimal cerebral blood flow in females versus males during old age. As reflective of the pattern of cerebral blood flow decline in human subjects, inward-rectifying K+ (KIR) channel function decreased with progressive age regardless of sex. Combined age-related analyses masked male versus female aging and, contrary to expectation, hydrogen peroxide played a minimal role. Altogether, we conclude a sex-based divergence in cerebrovascular endothelial GPCR and K+ channel function while highlighting a previously unidentified form of age-related endothelial dysfunction as reduced KIR channel function. (10/2020) (link)
- Hakim MA & Behringer EJ (2020). Development of Alzheimer's disease progressively alters sex-dependent KCa and sex-independent KIR channel function in cerebrovascular endothelium. J Alzheimer’s Dis. 76(4):1423-1442. PMID: 32651315; PMCID: PMC7709862 Background: Development of Alzheimer's disease (AD) pathology is associated with impaired blood flow delivery of oxygen and nutrients throughout the brain. Cerebrovascular endothelium regulates vasoreactivity of blood vessel networks for optimal cerebral blood flow. Objective: We tested the hypothesis that cerebrovascular endothelial Gq-protein-coupled receptor (GPCR; purinergic and muscarinic) and K+ channel [Ca2+-activated (KCa2.3/SK3 and KCa3.1/IK1) and inward-rectifying (KIR2.x)] function declines during progressive AD pathology. Methods: We applied simultaneous measurements of intracellular Ca2+ ([Ca2+]i) and membrane potential (Vm) in freshly isolated endothelium from posterior cerebral arteries of 3×Tg-AD mice [young, no pathology (1- 2 mo), cognitive impairment (CI; 4- 5 mo), extracellular Aβ plaques (Aβ; 6- 8 mo), and Aβ plaques + neurofibrillary tangles (AβT; 12- 15 mo)]. Results: The coupling of ΔVm-to-Δ[Ca2+]i during AβT pathology was lowest for both sexes but, overall, ATP-induced purinergic receptor function was stable throughout AD pathology. SKCa/IKCa channel function itself was enhanced by ∼20% during AD (Aβ+ AβT) versus pre-AD (Young + CI) in males while steady in females. Accordingly, hyperpolarization-induced [Ca2+]i increases following SKCa/IKCa channel activation and Δ[Ca2+]i-to-ΔVm coupling was enhanced by ≥two-fold during AD pathology in males but not females. Further, KIR channel function decreased by ∼50% during AD conditions versus young regardless of sex. Finally, other than a ∼40% increase in females versus males during Aβ pathology, [Ca2+]i responses to the mitochondrial uncoupler FCCP were similar among AD versus pre-AD conditions. Conclusion: Altogether, AD pathology represents a condition of altered KCa and KIR channel function in cerebrovascular endothelium in a sex-dependent and sex-independent manner respectively. (07/2020) (link)
- Stoll S, Xi J, Ma B, Leimena C, Behringer EJ, Qin G, Qiu H (2019). The valosin-containing protein protects the heart against pathological Ca2+ overload by modulating Ca2+ uptake proteins. Toxicol Sci. pii: kfz164. PMID: 31368507; PMCID: PMC6760276 Stress-induced mitochondrial calcium (Ca2+) overload is a key cellular toxic effectors and a trigger of cardiomyocyte death during cardiac ischemic injury through the opening of mitochondrial permeability transition pore (mPTP). We previously found that the valosin-containing protein (VCP), an ATPase-associated protein, protects cardiomyocytes against stress-induced death and also inhibits mPTP opening in vitro. However, the underlying molecular mechanisms are not fully understood. Here, we tested our hypothesis that VCP acts as a novel regulator of mitochondrial Ca2+ uptake proteins and resists cardiac mitochondrial Ca2+ overload by modulating mitochondrial Ca2+ homeostasis. By using a cardiac-specific transgenic (TG) mouse model in which VCP is overexpressed by 3.5 folds in the heart compared to the wild type (WT) mouse, we found that, under the pathological extra-mitochondrial Ca2+ overload, Ca2+ entry into cardiac mitochondria was reduced in VCP TG mice compared to their little-matched WT mice, subsequently preventing mPTP opening and ATP depletion under the Ca2+ challenge. Mechanistically, overexpression of VCP in the heart resulted in post-translational protein degradation of the mitochondrial Ca2+ uptake protein 1 (MICU1), an activator of the mitochondria Ca2+ uniporter (MCU) that is responsible for mitochondrial calcium uptake. Together, our results reveal a new regulatory role of VCP in cardiac mitochondrial Ca2+ homeostasis and unlock the potential mechanism by which VCP confers its cardioprotection. (07/2019) (link)
- Behringer EJ & Hakim MA (2019). Functional interaction among KCa and TRP channels for cardiovascular physiology: modern perspectives on aging and chronic disease. Int J Mol Sci. 20(6): pii: E1380. PMID: 30893836; PMCID: PMC6471369 Effective delivery of oxygen and essential nutrients to vital organs and tissues throughout the body requires adequate blood flow supplied through resistance vessels. The intimate relationship between intracellular calcium ([Ca2+]i) and regulation of membrane potential (Vm) is indispensable for maintaining blood flow regulation. In particular, Ca2+-activated K? (KCa) channels were ascertained as transducers of elevated [Ca2+]i signals into hyperpolarization of Vm as a pathway for decreasing vascular resistance, thereby enhancing blood flow. Recent evidence also supports the reverse role for KCa channels, in which they facilitate Ca2+ influx into the cell interior through open non-selective cation (e.g., transient receptor potential; TRP) channels in accord with robust electrical (hyperpolarization) and concentration (~20,000-fold) transmembrane gradients for Ca2+. Such an arrangement supports a feed-forward activation of Vm hyperpolarization while potentially boosting production of nitric oxide. Furthermore, in vascular types expressing TRP channels but deficient in functional KCa channels (e.g., collecting lymphatic endothelium), there are profound alterations such as downstream depolarizing ionic fluxes and the absence of dynamic hyperpolarizing events. Altogether, this review is a refined set of evidence-based perspectives focused on the role of the endothelial KCa and TRP channels throughout multiple experimental animal models and vascular types. We discuss the diverse interactions among KCa and TRP channels to integrate Ca2+, oxidative, and electrical signaling in the context of cardiovascular physiology and pathology. Building from a foundation of cellular biophysical data throughout a wide and diverse compilation of significant discoveries, a translational narrative is provided for readers toward the treatment and prevention of chronic, age-related cardiovascular disease. (03/2019) (link)
- Hakim MA & Behringer EJ. Simultaneous measurements of intracellular calcium and membrane potential in freshly isolated and intact mouse cerebral endothelium. J Vis Exp. 143:e58832, 2019. PMID: 30735188; PMCID: PMC6506161 Cerebral arteries and their respective microcirculation deliver oxygen and nutrients to the brain via blood flow regulation. Endothelial cells line the lumen of blood vessels and command changes in vascular diameter as needed to meet the metabolic demand of neurons. Primary endothelial-dependent signaling pathways of hyperpolarization of membrane potential (Vm) and nitric oxide typically operate in parallel to mediate vasodilation and thereby increase blood flow. Although integral to coordinating vasodilation over several millimeters of vascular length, components of endothelium-derived hyperpolarization (EDH) have been historically difficult to measure. These components of EDH entail intracellular Ca2+ [Ca2+]i increases and subsequent activation of small- and intermediate conductance Ca2+-activated K+ (SKCa/IKCa) channels. Here, we present a simplified illustration of the isolation of fresh endothelium from mouse cerebral arteries; simultaneous measurements of endothelial [Ca2+]i and Vm using Fura-2 photometry and intracellular sharp electrodes, respectively; and a continuous superfusion of salt solutions and pharmacological agents under physiological conditions (pH 7.4, 37 °C). Posterior cerebral arteries from the Circle of Willis are removed free of the posterior communicating and the basilar arteries. Enzymatic digestion of cleaned posterior cerebral arterial segments and subsequent trituration facilitates removal of adventitia, perivascular nerves, and smooth muscle cells. Resulting posterior cerebral arterial endothelial "tubes" are then secured under a microscope and examined using a camera, photomultiplier tube, and one to two electrometers while under continuous superfusion. Collectively, this method can simultaneously measure changes in endothelial [Ca2+]i and Vm in discrete cellular locations, in addition to the spreading of EDH through gap junctions up to millimeter distances along the intact endothelium. This method is expected to yield a high-throughput analysis of the cerebral endothelial functions underlying mechanisms of blood flow regulation in the normal and diseased brain. (01/2019) (link)
- Hakim MA, Buchholz JN, Behringer EJ (2018). Electrical dynamics of isolated cerebral and skeletal muscle endothelial tubes: differential roles of G-Protein coupled receptors and K+ channels. Pharmacol Res Perspect. 6(2), e00391. PMID: 29636977; PMCID: PMC5889193 Electrical dynamics of freshly isolated cerebral endothelium have not been determined independently of perivascular nerves and smooth muscle. We tested the hypothesis that endothelium of cerebral and skeletal muscle arteries differentially utilizes purinergic and muscarinic signaling pathways to activate endothelium-derived hyperpolarization. Changes in membrane potential (Vm) were recorded in intact endothelial tubes freshly isolated from posterior cerebral and superior epigastric arteries of male and female C57BL/6 mice (age: 3-8 months). Vm was measured in response to activation of purinergic (P2Y) and muscarinic (M3) receptors in addition to small- and intermediate-conductance Ca2+-activated K+ (SKCa/IKCa) and inward rectifying K+ (KIR) channels using ATP (100 μmol·L-1), acetylcholine (ACh; 10 μmol·L-1), NS309 (0.01-10 μmol·L-1), and 15 mmol·L-1 KCl, respectively. Intercellular coupling was demonstrated via transfer of propidium iodide dye and electrical current (±0.5-3 nA) through gap junctions. With similarities observed across gender, peak hyperpolarization to ATP and ACh in skeletal muscle endothelial tubes was ~twofold and ~sevenfold higher, respectively, vs cerebral endothelial tubes, whereas responses to NS309 were similar (from resting Vm ~-30 mV to maximum ~-80 mV). Hyperpolarization (~8 mV) occurred during 15 mmol·L-1 KCl treatment in cerebral but not skeletal muscle endothelial tubes. Despite weaker hyperpolarization during endothelial GPCR stimulation in cerebral vs skeletal muscle endothelium, the capability for robust SKCa/IKCa activity is preserved across brain and skeletal muscle. As vascular reactivity decreases with aging and cardiovascular disease, endothelial K+ channel activity may be calibrated to restore blood flow to respective organs regardless of gender. (04/2018) (link)
- Kapela A, Behringer EJ, Segal SS, Tsoukias NM (2018). Biophysical properties of microvascular endothelium: Requirements for initiating and conducting electrical signals. Microcirculation. 25(2). PMID: 29117630; PMCID: PMC5809195 OBJECTIVE: Electrical signaling along the endothelium underlies spreading vasodilation and blood flow control. We use mathematical modeling to determine the electrical properties of the endothelium and gain insight into the biophysical determinants of electrical conduction. METHODS: Electrical conduction data along endothelial tubes (40 μm wide, 2.5 mm long) isolated from mouse skeletal muscle resistance arteries were analyzed using cable equations and a multicellular computational model. RESULTS: Responses to intracellular current injection attenuate with an axial length constant (λ) of 1.2-1.4 mm. Data were fitted to estimate the axial (ra ; 10.7 MΩ/mm) and membrane (rm ; 14.5 MΩ·mm) resistivities, EC membrane resistance (Rm ; 12 GΩ), and EC-EC coupling resistance (Rgj ; 4.5 MΩ) and predict that stimulation of ≥30 neighboring ECs is required to elicit 1 mV of hyperpolarization at distance = 2.5 mm. Opening Ca2+ -activated K+ channels (KCa ) along the endothelium reduced λ by up to 55%. CONCLUSIONS: High Rm makes the endothelium sensitive to electrical stimuli and able to conduct these signals effectively. Whereas the activation of a group of ECs is required to initiate physiologically relevant hyperpolarization, this requirement is increased by myoendothelial coupling and KCa activation along the endothelium inhibits conduction by dissipating electrical signals. (02/2018) (link)
- Behringer EJ*, Scallan JP, Jafarnejad M Castorena-Gonzalez JA, Zawieja SD, Moore Jr. JE, Davis MJ, and Segal SS (2017). Calcium and electrical dynamics in lymphatic endothelium. J Physiol. 595(24): 7347-7368. *Co-first authorship. PMID: 28994159; PMCID: PMC5730853. Comment in “Endothelial tubes: another window into lymphatic function” by Kim A. Dora and Dirk F. Van Helden. J Physiol. 595(24):7267-7268, 2017. KEY POINTS: Endothelial cell function in resistance arteries integrates Ca2+ signalling with hyperpolarization to promote relaxation of smooth muscle cells and increase tissue blood flow. Whether complementary signalling occurs in lymphatic endothelium is unknown. Intracellular calcium and membrane potential were evaluated in endothelial cell tubes freshly isolated from mouse collecting lymphatic vessels of the popliteal fossa. Resting membrane potential measured using intracellular microelectrodes averaged ∼-70 mV. Stimulation of lymphatic endothelium by acetylcholine or a TRPV4 channel agonist increased intracellular Ca2+ with robust depolarization. Findings from Trpv4-/- mice and with computational modelling suggest that the initial mobilization of intracellular Ca2+ leads to influx of Ca2+ and Na+ through TRPV4 channels to evoke depolarization. Lymphatic endothelial cells lack the Ca2+ -activated K+ channels present in arterial endothelium to generate endothelium-derived hyperpolarization. Absence of this signalling pathway with effective depolarization may promote rapid conduction of contraction along lymphatic muscle during lymph propulsion. ABSTRACT: Subsequent to a rise in intracellular Ca2+ ([Ca2+ ]i ), hyperpolarization of the endothelium coordinates vascular smooth muscle relaxation along resistance arteries during blood flow control. In the lymphatic vasculature, collecting vessels generate rapid contractions coordinated along lymphangions to propel lymph, but the underlying signalling pathways are unknown. We tested the hypothesis that lymphatic endothelial cells (LECs) exhibit Ca2+ and electrical signalling properties that facilitate lymph propulsion. To study electrical and intracellular Ca2+ signalling dynamics in lymphatic endothelium, we excised collecting lymphatic vessels from the popliteal fossa of mice and removed their muscle cells to isolate intact LEC tubes (LECTs). Intracellular recording revealed a resting membrane potential of ∼-70 mV. Acetylcholine (ACh) increased [Ca2+ ]i with a time course similar to that observed in endothelium of resistance arteries (i.e. rapid initial peak with a sustained 'plateau'). In striking contrast to the endothelium-derived hyperpolarization (EDH) characteristic of arteries, LECs depolarized (>15 mV) to either ACh or TRPV4 channel activation. This depolarization was facilitated by the absence of Ca2+ -activated K+ (KCa ) channels as confirmed with PCR, persisted in the absence of extracellular Ca2+ , was abolished by LaCl3 and was attenuated ∼70% in LECTs from Trpv4-/- mice. Computational modelling of ion fluxes in LECs indicated that omitting K+ channels supports our experimental results. These findings reveal novel signalling events in LECs, which are devoid of the KCa activity abundant in arterial endothelium. Absence of EDH with effective depolarization of LECs may promote the rapid conduction of contraction waves along lymphatic muscle during lymph propulsion. (12/2017) (link)
- Behringer EJ* and Segal SS (2017). Impact of aging on calcium signaling and membrane potential in endothelium of resistance arteries: Role for mitochondria. J Gerontol A Biol Sci Med Sci. 72(12), 1627-1637. *Corresponding author. PMID: 28510636; PMCID: PMC5861896 The integral role of the endothelium during the coordination of blood flow throughout vascular resistance networks has been recognized for several decades now. Early examination of the distinct anatomy and physiology of the endothelium as a signaling conduit along the vascular wall has prompted development and application of an intact endothelial "tube" study model isolated from rodent skeletal muscle resistance arteries. Vasodilatory signals such as increased endothelial cell (EC) Ca2+ ([Ca2+ ]i ) and hyperpolarization take place in single ECs while shared between electrically coupled ECs through gap junctions up to distances of millimeters (≥2 mm). The small- and intermediate-conductance Ca2+ activated K+ (SKCa /IKCa or KCa 2.3/KCa 3.1) channels function at the interface of Ca2+ signaling and hyperpolarization; a bidirectional relationship whereby increases in [Ca2+ ]i activate SKCa /IKCa channels to produce hyperpolarization and vice versa. Further, the spatial domain of hyperpolarization among electrically coupled ECs can be finely tuned via incremental modulation of SKCa /IKCa channels to balance the strength of local and conducted electrical signals underlying vasomotor activity. Multifunctional properties of the voltage-insensitive SKCa /IKCa channels of resistance artery endothelium may be employed for therapy during the aging process and development of vascular disease. (11/2017) (link)
- Behringer EJ (2017). Calcium and electrical signaling in arterial endothelial tubes: New insights into cellular physiology and cardiovascular function. Microcirculation 24(3). PMID: 27801542; PMCID: PMC5404991 The integral role of the endothelium during the coordination of blood flow throughout vascular resistance networks has been recognized for several decades now. Early examination of the distinct anatomy and physiology of the endothelium as a signaling conduit along the vascular wall has prompted development and application of an intact endothelial "tube" study model isolated from rodent skeletal muscle resistance arteries. Vasodilatory signals such as increased endothelial cell (EC) Ca2+ ([Ca2+ ]i ) and hyperpolarization take place in single ECs while shared between electrically coupled ECs through gap junctions up to distances of millimeters (≥2 mm). The small- and intermediate-conductance Ca2+ activated K+ (SKCa /IKCa or KCa 2.3/KCa 3.1) channels function at the interface of Ca2+ signaling and hyperpolarization; a bidirectional relationship whereby increases in [Ca2+ ]i activate SKCa /IKCa channels to produce hyperpolarization and vice versa. Further, the spatial domain of hyperpolarization among electrically coupled ECs can be finely tuned via incremental modulation of SKCa /IKCa channels to balance the strength of local and conducted electrical signals underlying vasomotor activity. Multifunctional properties of the voltage-insensitive SKCa /IKCa channels of resistance artery endothelium may be employed for therapy during the aging process and development of vascular disease. (04/2017) (link)
- Behringer EJ and Segal SS (2015). Membrane potential governs calcium influx into microvascular endothelium: Integral role for muscarinic receptor activation. J Physiol. 593(20), 4531-4548. PMID: 26260126; PMCID: PMC4606535 In resistance arteries, coupling a rise of intracellular calcium concentration ([Ca(2+)]i) to endothelial cell hyperpolarization underlies smooth muscle cell relaxation and vasodilatation, thereby increasing tissue blood flow and oxygen delivery. A controversy persists as to whether changes in membrane potential (V(m)) alter endothelial cell [Ca(2+)]i. We tested the hypothesis that V(m) governs [Ca(2+)]i in endothelium of resistance arteries by performing Fura-2 photometry while recording and controlling V(m) of intact endothelial tubes freshly isolated from superior epigastric arteries of C57BL/6 mice. Under resting conditions, [Ca(2+)]i did not change when V(m) shifted from baseline (∼-40 mV) via exposure to 10 μM NS309 (hyperpolarization to ∼-80 mV), via equilibration with 145 mm [K(+)]o (depolarization to ∼-5 mV), or during intracellular current injection (±0.5 to 5 nA, 20 s pulses) while V(m) changed linearly between ∼-80 mV and +10 mV. In contrast, during the plateau (i.e. Ca(2+) influx) phase of the [Ca(2+)]i response to approximately half-maximal stimulation with 100 nm ACh (∼EC50), [Ca(2+)]i increased as V(m) hyperpolarized below -40 mV and decreased as V(m) depolarized above -40 mV. The magnitude of [Ca(2+)]i reduction during depolarizing current injections correlated with the amplitude of the plateau [Ca(2+)]i response to ACh. The effect of hyperpolarization on [Ca(2+)]i was abolished following removal of extracellular Ca(2+), was enhanced subtly by raising extracellular [Ca(2+)] from 2 mm to 10 mm and was reduced by half in endothelium of TRPV4(-/-) mice. Thus, during submaximal activation of muscarinic receptors, V(m) can modulate Ca(2+) entry through the plasma membrane in accord with the electrochemical driving force. (10/2015) (link)
- Socha MJ, Boerman EM, Behringer EJ, Shaw RL, Domeier TL, and Segal SS (2015). Advanced age protects microvascular endothelium from aberrant Ca2+ influx and cell death induced by hydrogen peroxide. J Physiol. 593(9), 2155-2169. PMID: 25689097; PMCID: PMC4422569 KEY POINTS: Calcium signalling in endothelial cells of resistance arteries is integral to blood flow regulation. Oxidative stress and endothelial dysfunction can prevail during advanced age and we questioned how calcium signalling may be affected. Intact endothelium was freshly isolated from superior epigastric arteries of Young (∼4 months) and Old (∼24 months) male C57BL/6 mice. Under resting conditions, with no difference in intracellular calcium levels, hydrogen peroxide (H2 O2 ) availability was ∼1/3 greater in endothelium of Old mice while vascular catalase activity was reduced by nearly half. Compared to Old, imposing oxidative stress (200 μm H2 O2 ) for 20 min increased intracellular calcium to 4-fold greater levels in endothelium of Young in conjunction with twice the calcium influx. Prolonged (60 min) exposure to H2 O2 induced 7-fold greater cell death in endothelium of Young. Microvascular adaptation to advanced age may protect endothelial cells during elevated oxidative stress to preserve functional viability of the intima. ABSTRACT: Endothelial cell Ca(2+) signalling is integral to blood flow control in the resistance vasculature yet little is known of how its regulation may be affected by advancing age. We tested the hypothesis that advanced age protects microvascular endothelium by attenuating aberrant Ca(2+) signalling during oxidative stress. Intact endothelial tubes (width, ∼60 μm; length, ∼1000 μm) were isolated from superior epigastric arteries of Young (3-4 months) and Old (24-26 months) male C57BL/6 mice and loaded with Fura-2 dye to monitor [Ca(2+) ]i . At rest there was no difference in [Ca(2+) ]i between age groups. Compared to Young, the [Ca(2+) ]i response to maximal stimulation with acetylcholine (3 μm, 2 min) was ∼25% greater in Old, confirming signalling integrity with advanced age. Basal H2 O2 availability was ∼33% greater in Old while vascular catalase activity was reduced by half. Transient exposure to elevated H2 O2 (200 μm, 20 min) progressively increased [Ca(2+) ]i to ∼4-fold greater levels in endothelium of Young versus Old. With no difference between age groups at rest, Mn(2+) quench of Fura-2 fluorescence revealed 2-fold greater Ca(2+) influx in Young during elevated H2 O2 ; this effect was attenuated by ∼75% using ruthenium red (5 μm) as a broad-spectrum inhibitor of transient receptor potential channels. Prolonged exposure to H2 O2 (200 μm, 60 min) induced ∼7-fold greater cell death in endothelium of Young versus Old. Thus, microvascular endothelium can adapt to advanced age by reducing Ca(2+) influx during elevated oxidative stress. Protection from cell death during oxidative stress will sustain endothelial integrity during ageing. (05/2015) (link)
- Behringer EJ, Shaw RL, Westcott EB, Socha MJ, and Segal SS (2013). Aging impairs electrical conduction along endothelium of resistance arteries through enhanced Ca2+-activated K+ channels activation. Arterioscler Thromb Vasc Biol. 33, 1892-1901. PMID: 23723370; PMCID: PMC3769416 OBJECTIVE: Intercellular conduction of electrical signals underlies spreading vasodilation of resistance arteries. Small- and intermediate-conductance Ca(2+)-activated K(+) channels of endothelial cells serve a dual function by initiating hyperpolarization and modulating electrical conduction. We tested the hypothesis that regulation of electrical signaling by small- and intermediate-conductance Ca(2+)-activated K(+) channels is altered with advancing age. APPROACH AND RESULTS: Intact endothelial tubes (60 µm wide; 1-3 mm long) were freshly isolated from male C57BL/6 mouse (Young: 4-6 months; Intermediate: 12-14 months; Old: 24-26 months) superior epigastric arteries. Using dual intracellular microelectrodes, current was injected (± 0.1-3 nA) at site 1 while recording membrane potential (Vm) at site 2 (separation distance: 50-2000 µm). Across age groups, greatest differences were observed between Young and Old. Resting Vm in Old (-38 ± 1 mV) was more negative (P<0.05) than Young (-30 ± 1 mV). Maximal hyperpolarization to both direct (NS309) and indirect (acetylcholine) activation of small- and intermediate-conductance Ca(2+)-activated K(+) channels was sustained (ΔVm ≈-40 mV) with age. The length constant (λ) for electrical conduction was reduced (P<0.05) from 1630 ± 80 µm (Young) to 1320 ± 80 µm (Old). Inhibiting small- and intermediate-conductance Ca(2+)-activated K(+) channels with apamin+charybdotoxin or scavenging hydrogen peroxide (H2O2) with catalase improved electrical conduction (P<0.05) in Old. Exogenous H2O2 (200 µmol/L) in Young evoked hyperpolarization and impaired electrical conduction; these effects were blocked by apamin+charybdotoxin. CONCLUSIONS: Enhanced current loss through Ca2+-activated K+ channel activation impairs electrical conduction along the endothelium of resistance arteries with aging. Attenuating the spatial domain of electrical signaling will restrict the spread of vasodilation and thereby contribute to blood flow limitations associated with advanced age. (08/2013) (link)
- Behringer EJ and Segal SS (2012). Spreading the signal for vasodilatation: Implications for skeletal muscle blood flow control and the effects of aging. J. Physiol. 590 (Pt 24), 6277-6284. PMID: 22890708; PMCID: PMC3533190 Blood flow control requires coordinated contraction and relaxation of smooth muscle cells (SMCs) along and among the arterioles and feed arteries that comprise vascular resistance networks. Whereas smooth muscle contraction of resistance vessels is enhanced by noradrenaline release along perivascular sympathetic nerves, the endothelium is integral to coordinating smooth muscle relaxation. Beyond producing nitric oxide in response to agonists and shear stress, endothelial cells (ECs) provide an effective conduit for conducting hyperpolarization along vessel branches and into surrounding SMCs through myoendothelial coupling. In turn, bidirectional signalling from SMCs into ECs enables the endothelium to moderate adrenergic vasoconstriction in response to sympathetic nerve activity. This review focuses on the endothelium as the cellular pathway that coordinates spreading vasodilatation. We discuss the nature and regulation of cell-to-cell coupling through gap junctions, bidirectional signalling between ECs and SMCs, and how oxidative stress during ageing may influence respective signalling pathways. Our recent findings illustrate the role of small (SK(Ca)) and intermediate (IK(Ca)) Ca(2+) activated K(+) channels as modulators of electrical conduction along the endothelium. Gaps in current understanding indicate the need to determine mechanisms that regulate intracellular Ca(2+) homeostasis and ion channel activation in the resistance vasculature with advancing age. (12/2012) (link)
- Socha MJ, Domeier TL, Behringer EJ, Segal SS (2012). Coordination of intercellular Ca2+ signaling in endothelial cell tubes of resistance arteries. Microcirculation. 19(8), 757-770. PMID: 22860994; PMCID: PMC3502682 OBJECTIVE: To test the hypothesis that Ca(2+) responses to GPCR activation are coordinated between neighboring ECs of resistance arteries. METHODS: EC tubes were freshly isolated from superior epigastric arteries of C57BL/6 mice. Intercellular coupling was tested using microinjection of propidium iodide. Following loading with fluo-4 dye, intracellular Ca(2+) responses to ACh were imaged with confocal microscopy. RESULTS: Cell-to-cell transfer of propidium iodide confirmed functional GJCs. A 1 μm ACh stimulus evoked Ca(2+) responses (9.8 ± 0.8/min, F/F(0) = 3.11 ± 0.2) which pseudo-line-scan analysis revealed as composed of Ca(2+) waves and spatially restricted Ca(2+) release events. A 100 nm ACh stimulus induced Ca(2+) responses of lower frequency (4.5 ± 0.7/min) and amplitude (F/F(0) = 1.95 ± 0.11) composed primarily of spatially restricted events. The time interval between Ca(2+) waves in adjacent cells (0.79 ± 0.12 s) was shorter (p < 0.05) than that between nonadjacent cells (1.56 ± 0.25 s). Spatially restricted Ca(2+) release events had similar frequencies and latencies between adjacent and nonadjacent cells. Inhibiting intracellular Ca(2+) release with 2-APB, Xestospongin C or thapsigargin eliminated Ca(2+) responses. CONCLUSIONS: With moderate GPCR stimulation, localized Ca(2+) release events predominate among cells. Greater GPCR stimulation evokes coordinated intercellular Ca(2+) waves via the ER. Calcium signaling during GPCR activation is complex among cells, varying with stimulus intensity and proximity to actively signaling cells. (11/2012) (link)
- Behringer EJ, Socha MJ, Polo-Parada L, Segal SS (2012). Electrical conduction along endothelial cell tubes from mouse feed arteries: confounding actions of glycyrrhetinic acid derivatives. Br J Pharmacol. 166(2), 774-787. PMID: 22168386; PMCID: PMC3417504 BACKGROUND AND PURPOSE: Electrical conduction along endothelium of resistance vessels has not been determined independently of the influence of smooth muscle, surrounding tissue or blood. Two interrelated hypotheses were tested: (i) Intercellular conduction of electrical signals is manifest in endothelial cell (EC) tubes; and (ii) Inhibitors of gap junction channels (GJCs) have confounding actions on EC electrical and Ca(2+) signalling. EXPERIMENTAL APPROACH: Intact EC tubes were isolated from abdominal muscle feed (superior epigastric) arteries of C57BL/6 mice. Hyperpolarization was initiated with indirect (ACh) and direct (NS309) stimulation of intermediate- and small-conductance Ca(2+) -activated K(+) channels (IK(Ca) /SK(Ca) ). Remote membrane potential (V(m) ) responses to intracellular current injection defined the length constant (λ) for electrical conduction. Dye coupling was evaluated following intracellular microinjection of propidium iodide. Intracellular Ca(2+) dynamics were determined using Fura-2 photometry. Carbenoxolone (CBX) or β-glycyrrhetinic acid (βGA) was used to investigate the role of GJCs. KEY RESULTS: Steady-state V(m) of ECs was -25 mV. ACh and NS309 hyperpolarized ECs by -40 and -60 mV respectively. Electrical conduction decayed monoexponentially with distance (λ∼1.4 mm). Propidium iodide injected into one EC spread into surrounding ECs. CBX or βGA inhibited dye transfer, electrical conduction and EC hyperpolarization reversibly. Both agents elevated resting Ca(2+) while βGA inhibited responses to ACh. CONCLUSIONS AND IMPLICATIONS: Individual cells were effectively coupled to each other within EC tubes. Inhibiting GJCs with glycyrrhetinic acid derivatives blocked hyperpolarization mediated by IK(Ca) /SK(Ca) channels, regardless of Ca(2+) signalling, obviating use of these agents in distinguishing key determinants of electrical conduction along the endothelium. (05/2012) (link)
- Behringer EJ and Segal SS (2012). Tuning electrical conduction along endothelial cell tubes through Ca2+-activated K+ channels. Circ Res. 110, 1311-1321. PMID: 22492531; PMCID: PMC3467972 RATIONALE: Electrical conduction through gap junction channels between endothelial cells of resistance vessels is integral to blood flow control. Small and intermediate-conductance Ca(2+)-activated K(+) channels (SK(Ca)/IK(Ca)) initiate electrical signals in endothelial cells, but it is unknown whether SK(Ca)/IK(Ca) activation alters signal transmission along the endothelium. OBJECTIVE: We tested the hypothesis that SK(Ca)/IK(Ca) activity regulates electrical conduction along the endothelium of resistance vessels. METHODS AND RESULTS: Freshly isolated endothelial cell tubes (60 μm wide; 1-3 mm long; cell length, ≈35 μm) from mouse skeletal muscle feed (superior epigastric) arteries were studied using dual intracellular microelectrodes. Current was injected (±0.1-3 nA) at site 1 while recording membrane potential (V(m)) at site 2 (separation distance=50-2000 μm). SK(Ca)/IK(Ca) activation (NS309, 1 μmol/L) reduced the change in V(m) along endothelial cell tubes by ≥50% and shortened the electrical length constant (λ) from 1380 to 850 μm (P<0.05) while intercellular dye transfer (propidium iodide) was maintained. Activating SK(Ca)/IK(Ca) with acetylcholine or SKA-31 also reduced electrical conduction. These effects of SK(Ca)/IK(Ca) activation persisted when hyperpolarization (>30 mV) was prevented with 60 mmol/L [K(+)](o). Conversely, blocking SK(Ca)/IK(Ca) (apamin+charybdotoxin) depolarized cells by ≈10 mV and enhanced electrical conduction (ie, changes in V(m)) by ≈30% (P<0.05). CONCLUSIONS: These findings illustrate a novel role for SK(Ca)/IK(Ca) activity in tuning electrical conduction along the endothelium of resistance vessels by governing signal dissipation through changes in membrane resistance. Voltage-insensitive ion channels can thereby tune intercellular electrical signaling independent from gap junction channels. (05/2012) (link)
- Socha MJ*, Behringer EJ*, Segal SS. (2012). Calcium and electrical signaling along endothelium of the resistance vasculature. Basic Clin Pharmacol Toxicol. 110(1), 80-86. *Co-first authorship PMID: 21917120; PMCID: PMC3271116 This MiniReview is focused on the nature of intercellular signalling along the endothelium that helps to co-ordinate blood flow control in vascular resistance networks. Vasodilation initiated by contracting skeletal muscle ascends from arterioles within the tissue to encompass resistance arteries upstream and thereby increase blood flow during exercise. In resistance vessels, acetylcholine microiontophoresis or intracellular current injection initiates hyperpolarization that conducts through gap junction channels (GJCs) along the vessel wall resulting in conducted vasodilation (CVD). Both ascending vasodilation and CVD are eliminated with endothelial cell (EC) disruption, pointing to common signalling events and mutual dependence upon EC integrity. As demonstrated by electrical coupling and dye transfer during intracellular recording, their longitudinal orientation and robust expression of GJCs enable ECs to play a predominant role in CVD. Once conduction is initiated, a major interest centres on whether CVD is purely passive or involves additional 'active' signalling events. Here, we discuss components for Ca²? and electrical signalling with an emphasis on intercellular coupling through endothelial GJCs. We stress the importance of understanding relationships between intracellular Ca²? dynamics, EC hyperpolarization and CVD while integrating findings from isolated ECs into more complex interactions in vivo. Whereas endothelial dysfunction accompanies cardiovascular disease and the components of intra- and inter-cellular signalling are increasingly well defined, little is known of how Ca²? signalling and electrical conduction along microvascular endothelium are altered in diseased states. Thus, greater insight into how these relationships are governed and interact is a key goal for continued research efforts. (01/2012) (link)
- Behringer EJ, Leite LD, Buchholz NE, Keeney MG, Pearce WJ, Vanterpool CK, Wilson SM, Buchholz JN (2009). Maturation and long-term hypoxia alters Ca2+-induced Ca2+ release in sheep cerebrovascular sympathetic neurons. J Appl Physiol. 107(4), 1223-1234. PMID: 19644029; PMCID: PMC2763832 The contribution of sympathetic nerves arising from the superior cervical ganglia (SCG) toward the growth and function of cerebral blood vessels is pertinent throughout maturation as well as in response to cardiovascular stress imposed by high-altitude long-term hypoxia (LTH). The function of SCG sympathetic neurons is dependent on intracellular Ca2+ concentration ([Ca2+](i)) signaling, which is strongly influenced by a process known as Ca2+-induced Ca2+ release (CICR) from the smooth endoplasmic reticulum (SER). In this study, we used the sheep SCG neuronal model to test the hypotheses that maturation decreases CICR and high-altitude LTH depresses CICR in fetal SCG neurons but not in those of the adult. We found that the contribution of CICR to electric field stimulation (EFS)-evoked [Ca2+] i transients was greatest in SCG cells from normoxic fetuses and was abolished by LTH. The decline in CICR was associated with a reduction in sarco(endo) plasmic reticulum Ca2+-ATPase (SERCA) function in fetal SCG cells during LTH, reducing SER Ca2+ levels below the threshold needed for the coupling of Ca2+ influx and CICR. With respect to the maturation from the fetus to adult, the decrease in CICR may reflect both a reduction in the levels of ryanodine receptor isoforms 2 and 3 and SERCA function. In response to LTH and in contrast to the fetus, CICR function in adult SCG cells is maintained and may reflect alterations in other mechanisms that modulate the CICR process. As CICR is instrumental in the function of sympathetic neurons within the cerebrovasculature, the loss of this signaling mechanism in the fetus may have consequences for the adaptation to LTH in terms of fetal susceptibility to vascular insults. (07/2009) (link)
- Behringer EJ, Vanterpool CK, Pearce WJ, Wilson SM, & Buchholz JN (2009). Advancing Age Alters the Contribution of Calcium Release From Smooth Endoplasmic Reticulum Stores in Superior Cervical Ganglion Cells. J Gerontol A Biol Sci Med Sci. 64(1), 34-44. PMID: 19196634; PMCID: PMC2673896 In superior cervical ganglion (SCG) neurons calcium-induced calcium release (CICR), mediated by ryanodine receptors (RyRs), contributes to stimulation-evoked intracellular calcium ([Ca(2+)](i)) transients. Hypothesis: The contribution of CICR to electrical field stimulation (EFS)-evoked [Ca(2+)](i) transients in SCG cells declines with senescence and may be partially recovered in the presence of caffeine. We measured EFS-evoked [Ca(2+)](i) transients in isolated fura-2-loaded SCG cells from Fischer-344 rats aged 6, 12, and 24 months with either the RyR antagonist ryanodine to block the contribution of CICR to [Ca(2+)](i) transients or caffeine to sensitize CICR to EFS. EFS-evoked [Ca(2+)](i) transients increased from 6 to 12 months and declined at 24 months and ryanodine decreased [Ca(2+)](i) transients in SCG cells from 6- and 12-monthold animals only. Caffeine significantly increased EFS-evoked [Ca(2+)](i) transients in all age groups. These data suggest that CICR declines with senescence and residual CICR function may be reclaimed in senescent cells with caffeine. (01/2009) (link)
- Buchholz JN, Behringer EJ, Pottorf BJ, Pearce WJ and Vanterpool CK (2007). Age–dependent changes in Ca2+ homeostasis in peripheral neurons: implications for changes in function. Aging Cell. 6(3), 285-296. PMID: 17517039; PMCID: PMC1974774 Calcium ions represent universal second messengers within neuronal cells integrating multiple cellular functions, such as release of neurotransmitters, gene expression, proliferation, excitability, and regulation of cell death or apoptotic pathways. The magnitude, duration and shape of stimulation-evoked intracellular calcium ([Ca2+]i) transients are determined by a complex interplay of mechanisms that modulate stimulation-evoked rises in [Ca2+]i that occur with normal neuronal function. Disruption of any of these mechanisms may have implications for the function and health of peripheral neurones during the aging process. This review focuses on the impact of advancing age on the overall function of peripheral adrenergic neurones and how these changes in function may be linked to age-related changes in modulation of [Ca2+]i regulation. The data in this review suggest that normal aging in peripheral autonomic neurones is a subtle process and does not always result in dramatic deterioration in their function. We present studies that support the idea that in order to maintain cell viability peripheral neurones are able to compensate for an age-related decline in the function of at least one of the neuronal calcium-buffering systems, smooth endoplasmic reticulum calcium ATPases, by increased function of other calcium-buffering systems, namely, the mitochondria and plasmalemma calcium extrusion. Increased mitochondrial calcium uptake may represent a 'weak point' in cellular compensation as this over time may contribute to cell death. In addition, we present more recent studies on [Ca2+]i regulation in the form of the modulation of release of calcium from smooth endoplasmic reticulum calcium stores. These studies suggest that the contribution of the release of calcium from smooth endoplasmic reticulum calcium stores is altered with age through a combination of altered ryanodine receptor levels and modulation of these receptors by neuronal nitric oxide containing neurones. (06/2007) (link)
Books and Chapters
- Buchholz JN, Behringer EJ (Editors). Calcium and Signal Transduction. Physiology Series, Volume 1. London, UK: Intech Open; 2019:1-192. ISBN: 978-1-78984-249-4. Since the development of microelectronic clamping methodology and fluorescent indicators for direct measurement of dynamic intracellular calcium transients, our understanding of biological signal transduction has progressed dramatically since the 1980s. Calcium is a universal signal in biology that modulates gene expression, transmitter and hormone release, muscular movement, and even "programmed" cell death. This book represents a compilation of chapters from a diverse set of expert biologists throughout the world who have conducted research in the general area of calcium signaling in organisms ranging from bacteria to humans. In accord with priorities of resolving human disease, the reader will also benefit from learning calcium's role in cellular signaling pathology relating to acute or chronic conditions such as vomiting, sepsis, obesity, hypertension, and cancer. (01/2018) (link)
- Behringer EJ, Segal SS. Ion channels in control of blood flow: electrical conduction along endothelium of resistance arteries. In: Vascular Ion Channels in Physiology and Disease. Cham, Switzerland: Springer; 2016:79–100. ISBN: 978-3319296333. The regulation of tissue blood flow in response to the metabolic demand of parenchymal cells is effected through changes in vascular resistance as governed by arteriolar networks and their proximal feed arteries. Vasodilation and vasoconstriction must be coordinated among downstream and upstream segments to optimize blood flow distribution within the tissue and to attain maximal perfusion of the vascular supply. Such coordinated vasomotor activity is promoted by the transmission of electrical signals (e.g., hyperpolarization and depolarization) through gap junctions from cell-to-cell along the vessel wall. Based upon underlying structural and functional relationships, we explore the biophysical basis of intercellular electrical signaling along the endothelium of resistance arteries. The endothelium is presented as a cable, whereby electrical signals decay passively with distance from the site of initiation. Key to our findings is how K+ channels expressed constitutively in endothelial cell membranes [e.g., KCa2.3 (SKCa) and KCa3.1 (IKCa)] regulate the spatial domain of electrical signal transmission and how this role is effected during advanced age through the actions of hydrogen peroxide. New insights into the regulation of electrical conduction along microvascular endothelium advance our understanding of how blood flow is governed by ion channels while providing mechanistic insight into how such processes can be affected during vascular disease. (01/2016) (link)
- Buchholz JN, Pottorf WJ, Vanterpool CK, Behringer EJ and Duckles SP (2012). Senescence, Chapter title: Calcium Regulation in Neuronal Function with Advancing Age: Limits of Homeostasis. Rijeka, Croatia: InTech; 2012: 531-558. ISBN: 978-953-308-28-6. Neurons are specialized excitable cells that transmit information to other neurons or to end effector cells such as skeletal muscle, heart muscle and blood vessel smooth muscle cells, maintaining posture, locomotion and cardiovascular function. Transmission of information from neurons to effector cells usually involves secretion of neurotransmitters contained in clustered pools of synaptic vesicles. This unique anatomical arrangement allows for rapid response to the stimulus of calcium influx and sustained release of neurotransmitters under low and higher frequency conditions (Peirbone et al., 1995; Siksou et al., 2011). Calcium is hypothesized to act as a universal second messenger in excitable cells; a large volume of literature spanning more than 30 years supports this idea. Calcium integrates multiple neuronal cell functions including initiation of neurotransmitter release, regulation of gene expression, proliferation, excitability and plasticity, and activation of cell death pathways in apoptosis (Malenka et al., 1989; Choi, 1992; Berridge, 1995, 1998; Clapham, 1995; Ginty, 1997; Wuytack et al., 2002; Cavazzini et al., 2005). In resting neurons a large electrochemical gradient of approximately 10,000-fold exists between the extracellular environment and the cytosol; this physical arrangement allows for rapid activation of transmitter release via mobilization of release vesicles. In peripheral neurons including sympathetic neurons, calcium signaling begins with rapid opening of voltage-gated L, N and some R type calcium channels allowing calcium to enter the cytosol (Kostyuk, 1989; Kostyuk et al., 1993; Trouslard et al., 1993; Vanterpool et al., 2005). More recently the nomenclature of L, N and R type channels has taken on increased complexity due to definition of differences in their activation voltages, coding genes and hence amino acid sequences of the ?1-subunits that comprise the channel pore (Catterall et al., 2005). For example L and N type channels have been divided into five groups: Cav1.1. Cav 1.2, Cav 1.3 and Cav 1.4 (L-type) and Cav 2.2 (N-type). R type channels, originally termed "residual" because they are resistant to dihidropyridines, which block L-type channels and omega conotoxin, which blocks N-type channels (Catteral et al., 2005), are now denoted as Cav 2.3. Given the importance of precise neuronal signaling and the need for regulatory mechanisms to sustain efficient signaling, a number of additional cellular mechanisms play a critical role in modulating cellular calcium. These complex calcium regulatory mechanisms are illustrated in figure 1(A). Following the activation of calcium influx through voltage-gated calcium channels, much of the calcium increase is immediately dampened by multiple calcium buffering proteins (Dove et al., 2000). Despite this rapid calcium buffering, functional signaling is sustained by rapid release of calcium from smooth endoplasmic reticulum (SER) stores. This process has been termed calcium-induced calcium release (CICR) and is mediated by calcium activation of ryanodine receptor (RyR) channels (Belan et al., 1993; Verkhratsky & Shmigol, 1996; Usachev & Thayer, 1997, 1999a,b; Verkhratsky & Petersen, 1998; Akita & Kuba, 2000; Berridge 2002; Behringer et al., 2009a). A variety of additional calcium buffering systems can be activated by a rise in intracellular calcium ([Ca2+]i), depending on both the magnitude and duration of the [Ca2+]i transient. Buffering systems include calcium-buffering proteins, energy dependent SER Ca2+ ATPases (SERCA), plasmalemmal Ca2+-ATPases (PMCA), mitochondrial Ca2+/H+ symporters and Na+/Ca2+-exchangers. All of these calcium buffering systems act to modulate the shape and magnitude of stimulus-evoked [Ca2+]i transients and contribute to restoration of [Ca2+]i levels (Werth & Thayer, 1994; Buchholz et al., 1996; Werthet al., 1996; Usachev & Thayer, 1999a; Pottorf et al ., 2000a,c, 2002; Wuytack et al., 2002). Furthermore, the SERCA function and the CICR process are interdependent, as SERCA pumps not only buffer [Ca2+]i transients but also refill SER calcium stores. This interdependence maintains CICR during repeated neuronal activation (Vanterpool et al., 2005). Disruption of any of these mechanisms with advancing age may result in altered function and health of peripheral neurons. This chapter will focus on the impact of advancing age, from young adult to senescence, on the function of adrenergic nerves and the mechanisms by which alterations in function may be related to age-related changes in modulation of [Ca2+]i with ongoing neuronal activity. Data from seminal studies on function of peripheral sensory and central neurons will also be included as important background for understanding the impact of age on adrenergic nerves. (01/2012) (link)